CGRP Antagonists: The Successors of the Triptans?
Dr. Axel Heinze, Dr. Katja Heinze-Kuhn and Prof. Dr. Hartmut Göbel 
Neurological-behavioral medicine pain clinic Kiel (https:// pain clinic.de)
The introduction of sumatriptan in migraine therapy not only changed migraine treatment significantly from 1991 onwards, but also provided the impetus for an unprecedented expansion of basic research. There are now 7 different triptans available that can still help patients with severe migraine attacks when all painkillers fail. But just as importantly, our understanding of migraines has increased immensely over the last 20 years. Medicine not only uses triptans successfully, it also knows their mechanism of action.
And yet there are patients who have not benefited from the progress of triptans. Basically, there are 3 possible reasons for this in individual cases:
1. Ineffectiveness of even the most potent triptans
2. Intolerance to even the mildest triptans
3. Presence of contraindications to the use of triptans
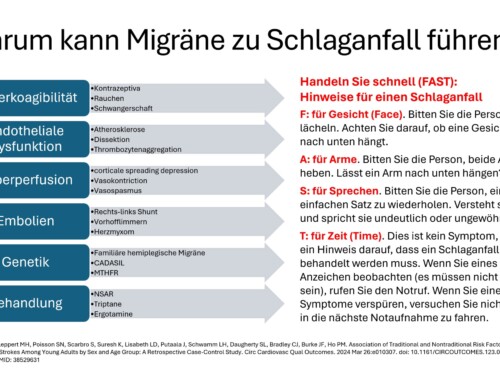
a. Reasonable suspicion or presence of any circulatory disorder
b. High blood pressure that cannot be adequately controlled.
c. Occurrence of pronounced and long-lasting migraine auras during the headache phase (e.g. in hemiplegic migraine or basilar type migraine)
The reason for these restrictions is the vasoconstricting effect of triptans , which particularly affects the blood vessels of the head. In addition, due to insufficient data, the use of triptans during pregnancy or breastfeeding is still not recommended.
There is therefore still a need for therapeutic alternatives to triptans for patients with severe migraine attacks. In October 2007, data on the effectiveness of a substance called MK-0974 for migraines were published for the first time. MK-0974 belongs to the group of CGRP antagonists, a group of drugs that promises to become a possible alternative to triptans.
In order to understand the mechanism of action of CGRP antagonists, one must take a look at today's understanding of what happens in the brain during a migraine.
Hereditary factors play a crucial role in the development of migraines More than 70% of those affected know first-degree family members (parents, siblings or children) who also suffer from migraines. Children of migraine sufferers have a 2 to 4-fold increased risk of developing migraines compared to their peers. Underlying genetic defects been identified for a subtype of migraine, familial hemiplegic migraine These are responsible for the hypersensitivity to a variety of internal and external stimuli, the so-called trigger factors . These include, among other things, disruptions to the sleep-wake rhythm, hormonal fluctuations, changes in blood sugar levels or current stress levels, unusual physical stress or odors, noise or flickering lights. This means that although the genetic predisposition to migraines is passed down through the generations, whether migraines actually occur in individual cases and, if so, how severe and how frequently, depends largely on environmental factors.
A sterile (i.e. not caused by pathogens) inflammation in the area of the blood vessels of the meninges is responsible for the actual migraine headache. This inflammation is caused by the nervous system itself; It is therefore referred to as neurogenic inflammation . The inflammation leads to hypersensitivity of pain receptors in the meninges. The simple pulsation of the blood vessels in the meninges becomes a hammering, throbbing migraine pain - any physical strain, even just bending over, leads to further intensification of the pain.
According to current knowledge, a protein that is released from nerve fibers of the trigeminal nerve activated during a migraine attack is crucial for the development of the inflammation: the CGRP ( calcitonin gene related peptide ). Elevated CGRP levels were detected in the venous blood of patients during a migraine attack as early as 1988. After the attack ends or after successful treatment with a triptan, the CGRP level returns to normal. The effect of triptans on migraines is probably due to the inhibition of the release of CGRP . This desired effect is mediated via a specific serotonin receptor, the 5-HT 1 D receptor. However, triptans also activate another serotonin receptor, the 5-HT 1 B receptor, which mediates the undesirable vasoconstrictor effect.
This is where the CGRP antagonists in. Without affecting serotonin receptors (and, for example, constricting blood vessels) like triptans, they directly block CGRP receptor . As a result, the CGRP released during the migraine attack does not find a free receptor to which it could bind and therefore cannot cause any damage. The development or maintenance of the inflammation is interrupted and the migraine symptoms subside.
The study published by Ho and colleagues in the journal Neurology showed that the CGRP antagonist MK-0974 can interrupt an acute migraine attack just as effectively as the proven rizatriptan
The tolerability of MK-0974 was good. No serious adverse events occurred. The most frequently reported side effects were nausea, dizziness and fatigue, i.e. symptoms that can also be migraine symptoms. Accordingly, these side effects were also found in the placebo group.
International studies are currently examining the effectiveness and tolerability of MK-0974 in long-term use. It remains to be seen to what extent the high expectations that have now been raised can actually be fulfilled.
cgrp-antagonists-dgs-journal-pain-therapy-09052009
More on the topic in the original
- Denekas T, Troltzsch M, Vater A, Klussmann S, Messlinger K (2006). Inhibition of stimulated meningeal blood flow by a calcitonin gene-related peptide binding mirror-image RNA oligonucleotide. Br J Pharmacol 148 :536–543. | Article | PubMed | ChemPort |
- Edvinsson L (2004). Blockade of CGRP receptors in the intracranial vasculature: a new target in the treatment of headache. Cephalalgia 24 : 611–622. | Article | PubMed | ChemPort |
- Edvinsson L, Nilsson E, Jansen-Olesen I (2007). Inhibitory effect of BIBN4096BS, a CGRP8-37, a CGRP antibody and an RNA-Spiegelmer on CGRP induced vasodilation in the perfused and non-perfused rat middle cerebral artery. Br J Pharmacol 150 :633–640. | Article | PubMed | ChemPort |
- Goadsby PJ, Edvinsson L (1993). The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol 33 :48–56. | Article | PubMed | ISI | ChemPort |
- Goadsby PJ, Lipton RB, Ferrari MD (2002). Migraine—current understanding and treatment. N Engl J Med 346 :257–270. | Article | PubMed | ISI | ChemPort |
- Ho TW, Mannix LK, Fan X, Assaid C, Furtek C, Jones CJ et al . (2008). Randomized controlled trial of an oral CGRP receptor antagonist, MK-0974, in acute treatment of migraine. Neurology 70 : 1304–1312. | Article | PubMed | ChemPort |
- Juhl L, Edvinsson L, Olesen J, Jansen-Olesen I (2007). Effect of two novel CGRP-binding compounds in a closed cranial window rat model. Eur J Pharmacol 567 : 117–124. | Article | PubMed | ChemPort |
- Lennerz JK, Ruhle V, Ceppa EP, Neuhuber WL, Bunnett NW, Grady EF et al . (2008). Calcitonin receptor-like receptor (CLR), receptor activity-modifying protein 1 (RAMP1), and calcitonin gene-related peptide (CGRP). Immunoreactivity in the rat trigeminovascular system: differences between peripheral and central CGRP receptor distribution. J Comp Neurol 507 : 1277–1299. | Article | PubMed | ChemPort |
- Levy D, Burstein R, Strassman AM (2005). Calcitonin gene-related peptide does not excite or sensitize meningeal nociceptors: implications for the pathophysiology of migraine. Ann Neurol 58 :698–705. | Article | PubMed | ChemPort |
- Olesen J, Diener HC, Husstedt IW, Goadsby PJ, Hall D, Meier U et al . (2004). Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N Engl J Med 350 : 1104–1110. | Article | PubMed | ISI | ChemPort |
- van den Maagdenberg AM, Haan J, Terwindt GM, Ferrari MD (2007). Migraine: gene mutations and functional consequences. Curr Opin Neurol 20 : 299–305. | Article | PubMed | ChemPort |
- Zeller J, Poulsen KT, Sutton JE, Abdiche YN, Collier S, Chopra R et al . (2008). CGRP function-blocking antibodies inhibit neurogenic vasodilation without affecting heart rate or arterial blood pressure in the rat. Br J Pharmacol 155 : 1093–1103 (this issue). | Article |






Hello!
The above-mentioned drug has barely entered the testing phase when the next drug is already being tested:
ADX10059 (tezampanel).
It is a glutamate antagonist. It is hoped to interrupt the migraine chain reaction and the migraine cycle. Source: http://headacheandmigrainenews.com/adx10059-another-drug-in-the-pipeline/
and http://www.addexpharma.com/key-indications/migraine/mglur5-migraine/
Further information will only be available in 2010 .
Greetings Peter Schwirkmann