Medication-induced headache (MIKS) is also called medication overuse headache (MOH). It can occur if painkillers for headaches are taken at least 10 days a month. In particular, people who suffer from primary headaches such as migraines and tension headaches are often affected by medication overuse headaches.
In medication overuse headache (MOH), there is the paradoxical situation that the use of pain and migraine medications has led to an increase in headaches and migraines.
Medication overuse headache can be viewed as a complication of headache treatment.
In principle, any medication that is used effectively for the acute treatment of migraines and tension headaches can itself trigger headaches if taken too frequently. The greatest risk lies with mixed painkillers and triptans. What is important here is not the dose of the medication used, but rather the frequency of use.
Taking pain medications or triptans too frequently – by definition more than 10 days a month – can lead to an increase in the frequency of headaches. At the same time, the effectiveness and duration of action of the previously successfully used attack medication decreases, which in turn leads to the medication being taken more frequently. This creates a vicious circle of more and more headaches and more and more headache medications.
Self-medication for headaches makes sense for known types of headaches, it saves time and can definitely be taken care of if the self-medication is effective. Typical examples are an occasional tension headache or a migraine attack that responds to self-medication. The focus of treatment should be substances such as aspirin, paracetamol or ibuprofen. These medications should be taken early in the attack and in sufficient doses. If there are accompanying symptoms such as nausea or vomiting, additional anti-nausea medication can be used. The most important rule in the area of self-medication is the 10-20 rule: Acute painkillers should be taken on fewer than 10 days per month, and no painkillers for headaches should be used on at least 20 days per month. The background to this rule is that if it is exceeded, a so-called medication overuse headache can occur. The headaches become more frequent, become longer, become more severe and the accompanying disorders can also become more severe. The frequency of headaches increases continuously and eventually, after a few months, a permanent headache can develop. If the 10-20 rule is followed, a corresponding protective limit is present.
Drug-induced headache occurs as a complication of treatment for primary headaches. As the frequency of use of acute medication increases, the frequency of headaches increases, and a so-called secondary headache, the headache caused by medication overuse, arises as a complication of the treatment. Typically the 10-20 rule is exceeded, the headache frequency increases, eventually reaching 12, 15, 20 or more days a month with acute medication and even more headache days. The only long-term effective strategy is to take a so-called medication break. The administration of medication is interrupted. A rebound headache occurs, a so-called setback headache. In this phase, patients are very severely impaired. It is therefore necessary that they receive concomitant medication that does not include medications commonly used in acute attacks. The administration of prednisolone can also be helpful. So-called antiemetics, anti-nausea drugs, are used to treat nausea and vomiting. For mild cases, outpatient therapy can be carried out; for severe cases, inpatient treatment is, according to current studies, significantly more effective than outpatient or day hospital treatment. After the transition headache has subsided, medication to prevent the primary headache must be established to avoid a relapse into medication overuse headache. We have initiated the nationwide headache treatment network for long-term care; regional doctors can continue the treatment for over a year in order to advise the patients and optimize and adapt the drug and non-drug prevention accordingly.
When it comes to headaches, experience and behavior play a crucial role. They arise in the central nervous system. The central nervous system not only regulates body mechanisms and purely physical functions, its main task is to enable experience and behavior, to condition and control regulations, motivation and emotions. Psychological mechanisms therefore play a crucial role in all pain. Pain is experienced in the cerebral cortex and brought to consciousness. Psychological conditions are therefore always weighed into pain and change and color the experience of pain. Therefore, psychological therapy procedures and psychological strategies for pain prevention play a central role in pain treatment. Mental illnesses that lead to headaches are, in particular, depression and so-called somatoform disorders; psychoses can also cause psychological headaches. Treatment is aimed entirely at the underlying condition of these so-called secondary psychiatric headaches. Otherwise, for all types of headaches, especially primary headaches, psychological factors must be taken into account during treatment. This starts with keeping a headache calendar, behavioral analysis, relaxation techniques, treating anxiety and depression related to the headache. Social conditions, partnership issues and other things must also be taken into account in the treatment.
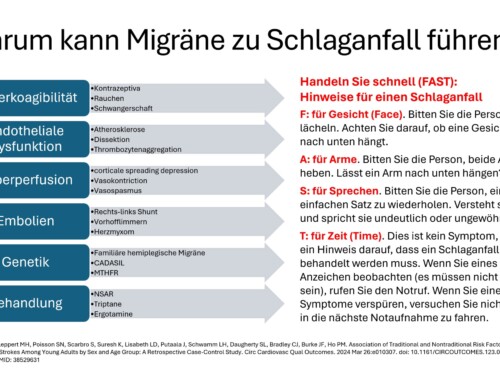
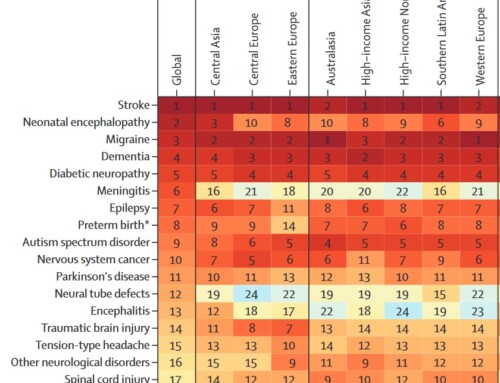
Today we distinguish between 363 different main headache diagnoses. There is no such thing as a “headache” or “a” stomach ache. The precise differentiation of the pain mechanisms and the conditions that maintain the pain is therefore of central importance. In the case of the most common headaches, migraines and tension-type headaches as well as medication overuse headaches, the mechanisms are now very well known, and it is therefore possible to specifically intervene in the pain mechanisms. Migraine pain is caused by a so-called neurogenic inflammation in the blood vessels of the meninges. Certain nerve messengers are released there, which cause local inflammation. This leads to increased sensitivity to pain in the vascular membranes, so every shock, every movement, every pulsation and throbbing hurts. The triggering of the excessive release of these inflammatory substances occurs through activation of certain nerve nuclei in the brain stem. This is a result of excessive regulation due to energy deficits due to increased energy turnover in the nerve cells. There are now 12 known risk genes for migraines. These lead to an amplification and release of the neurotransmitters and neuropeptides discussed in the nervous system. This means that migraine therapy must intervene in this process in a complex manner in order to stabilize the headache.
The development of headaches due to overuse of medication is explained by the exhaustion of the body's own pain defense system. Due to the frequent pain attacks and the excessive consumption of acute painkillers, the body's own pain defense system becomes increasingly exhausted and more and more headache episodes occur, up to a permanent headache at the end of the pathophysiological development.






Leave a comment