Digital care innovation with significant benefits for the future region of digital health (ZDG)

The Digital Health Future Region (ZDG) is an initiative of the Federal Ministry of Health planned to run until the end of 2022
This video explains to doctors how they can use the migraine app from the Kiel Pain Clinic and the Techniker Krankenkasse in professional care and how they can interpret the aggregated care analyzes for contemporary therapy adjustments. The film is designed in particular as a training film for the use of the migraine app in the future region of digital health (ZDG). The Digital Health Future Region is an initiative of the Federal Ministry of Health planned to run until the end of 2022. The aim of the Digital Health Future Region is to bring digital care solutions into greater practical application in the Berlin test region. In addition, knowledge should be gained about the use of digital care applications in the German healthcare system. Further information on the development of the future region can be found here .
Doctors play a crucial role in the success of the future region of digital health. As the direct contact and reference person for patients, they are crucial participants in the care process. If doctors want to keep up with digitalization in practice, they must be familiar with the migraine app and other digital care solutions, such as their blood pressure monitor or ECG. Only through in-depth training and skills can they implement technical innovations in everyday care. This makes innovative and modern diagnostics and treatment professionally possible in the care process. If you, as a doctor, would like to get involved as a ZDG doctor, you can find further information here. Find out how you can become a ZDG doctor or contact the office of the Digital Health Future Region for further details.

The aim of the Digital Health Future Region (ZDG) is to bring digital care solutions into greater practical application in the Berlin test region
The migraine app was developed in collaboration with doctors specializing in the treatment of migraine and headache patients in the nationwide headache treatment network, headache scientists, healthcare experts from the Techniker Krankenkasse and self-help groups. The iOS version was made available in October 2016, and an extension for the Apple Watch was released in December 2016. The Android version followed in February 2017. As of March 2020, there were a total of around 250,000 downloads. According to user numbers and reviews in the app stores, the migraine app, which is certified as a medical product, is the most widely used digital application in Germany to treat migraines and headaches. The migraine app is also the first app that is contractually integrated directly into the medical treatment and therapy within the framework of statutory health insurance via a care contract in accordance with Section 140a ff SGB V of the Techniker Krankenkasse for the integrated care of migraines and headaches [1-3] . The integration of the migraine app into the active care process leads to a demonstrable, significant benefit for patients and doctors [4].
Aggregated information, reporting, information and self-help tools
The digital care application documents the course of migraines and headaches with active data entry. It reports aggregated information from the data set and thus helps patients and the doctors in charge to monitor progress and success as well as adjust therapy. The migraine app contains reporting, information and self-help tools. It is registered as a Class I medical device. The concept focuses on professional involvement in the practical care of migraine and headache patients. The main goals are to make it easier to monitor progress and success, to increase adherence to therapy, to provide digital support and monitoring of treatment under medical guidance, to motivate therapy, and to provide information and knowledge about the clinical picture. In addition, those affected are digitally networked nationwide through self-help communities via a closed group on Facebook and the Headbook community, which at the same time creates a digital form of self-help group organization. This is now active as a registered association and is the largest self-help group on the subject in Germany.
The features of the migraine app

The migraine app helps patients with chronic headaches to accurately document the course of their illness digitally, analyze it and control it with just a few clicks
The migraine app helps patients with chronic headaches to accurately document the course of their illness digitally, analyze it and control it with just a few clicks. Table 1 provides an overview of the individual functions and the menu structure. The migraine app provides the user with feedback and information from the analyzed data. It suggests behavioral actions based on the individual data entered. For example, if the user exceeds the maximum permitted acute medication of a maximum of nine days per month, he or she will receive a warning. Extensive information and self-help tools are also available to patients. This allows them, among other things, to determine and reduce their risk of chronic disease, find a pain specialist nearby using a navigation tool or train progressive muscle relaxation in various versions under guidance. In expert live chats you can ask questions to headache experts and receive targeted answers.
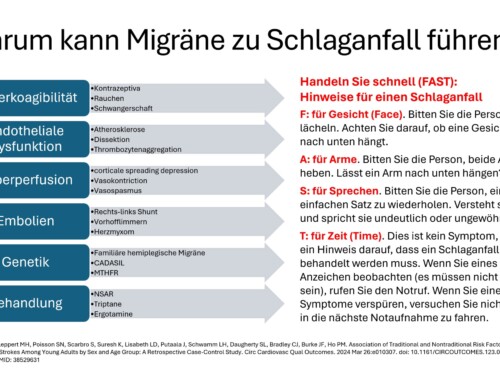
Digital orientation: migraine aura or stroke?
The migraine app also contains, among other things, the simulation of a migraine aura. It shows what visual disturbances look like during migraine attacks. Since the symptoms of a migraine aura are often confused with those of a stroke, those affected and doctors can make a quicker and easier differential diagnosis.
Migraine app use reduces headache and medication days

Using the migraine app is associated with a significant reduction in pain days by around 25% per month.
An extensive study [4] by the Kiel Pain Clinic and the Techniker Krankenkasse (TK) shows: Using the migraine app can significantly reduce pain days. On average, users of the migraine app suffer from headaches on around 25% fewer days per month than without using the app - on average 10 instead of 13.3 days per month. The study shows that patients benefit significantly from accompanying their treatment with the migraine app. You have fewer headache days per month and the need to take acute headache medication also decreases. For comparison: Most preventative headache medications reduce the number of headache days by an average of one to two days per month. The migraine app shows that scientifically based digital offerings in healthcare provide noticeable added value for individual patients and the insured community.
Around 10 million fewer headache days per year
Extrapolated to all users of the app, with currently around 250,000 downloads, the reduction in headache days can be estimated at around 10 million days per year in Germany. The study also shows that the app supports medical treatment and that digital medicine has arrived in modern medical consultations. Seven out of ten users surveyed (71%) bring the migraine app with them to the doctor. 58% use the app results to decide on therapy together with their doctor, especially to adjust medication. 76% say the app helps them stick to the treatment plan they created with their doctor. In addition, 80% prefer the app solution to a traditional paper pain diary.
Comparison of digital care with conventional care

The migraine app enables a data-based exchange about the impact of the pain disorder on an objective basis
The prerequisite for individually adapted and operationalized headache therapy is self-observation and documentation of the headache phenotype to monitor progress and success. Keeping a headache diary was therefore included early on in the guidelines for headache treatment [5]. A comparison of the possibilities of digital care with the migraine app with conventional care is shown in Table 2. Pain calendars and pain diaries on paper have a number of disadvantages. Information entry is static, data aggregation to support clinical decisions does not occur, documentation is limited and is often misplaced or forgotten. The use of apps in medicine is therefore one of the earliest professional applications of mobile computer technology. They were used early on to monitor the progress and success of pain and headache therapy [6-9]. Mobile software applications have a number of advantages over paper documentation. The smartphone is usually carried with you at all times and is the central communication device for over 80% of the population. The documentation of the headache phenotype and the course of the headache over time can be done immediately. Progress parameters can be entered directly into the app. Current information about environmental variables such as air temperature, air pressure and location can be automatically added digitally. The smartphone can generate aggregated, clear evaluations and reports from the data, which can be used directly to make treatment decisions and do not have to be counted out in a lengthy manner. Progression patterns can therefore be recognized directly and serve as a basis for further treatment in practice [10]. Monitoring progress and success using smartphone applications has proven to be more reliable than paper diaries. They show higher compliance compared to paper diaries [11], the compliance rate for electronic diaries is 94%, while for paper diaries it is only 11% [12].
Communication with patients during pain consultations is one of the core tasks of the doctor and the practice team in practical care. The migraine app enables a committed exchange about the impact of the pain disorder based on objective data. Communication based on the migraine app shows the patient that their concerns are being taken into account and that the doctor is keeping pace with contemporary developments in care. Doctors and patients can listen, ask questions and exchange information based on an objective analysis of the migraine app.

Quantitative course parameters make it possible for patients and doctors to optimize the therapy adjustment, monitor the course and increase the effectiveness of the treatment measure.
The migraine app strengthens the communicative skills of the doctor and the patient based on data. It enables a patient-oriented conversation and the development of a relationship of trust. The doctor can explain things in a comprehensible manner and encourage the patient to ask questions. Misunderstandings can be eliminated or prevented. The migraine app supports comprehensibility through knowledge and information. The doctor can express himself clearly and avoid technical vocabulary.
The digital application also saves time through aggregated, valid data that can be used immediately to make decisions that the patient can understand. The migraine app involves the patient in the treatment decision through transparency of the course and the success of the therapy so far.
Shared use by doctor and patient
Using quantitative progress parameters, it is possible for patients and doctors to optimize the therapy adjustment, control the progress and increase the effectiveness of the treatment measure. For this purpose, the consultation checklist was integrated into the migraine app. It can be accessed directly via the app's overview page by the patient or doctor in the cockpit (Figure 1 and Figure 2). Here you can find the consultation hour checklist with the summarized data sets for the current year and the previous year. This analysis can be exported as a PDF form, for example via email, and integrated into the doctor's practice information system. Storage of the data in the electronic patient file can also be made possible. Data retrieval can only take place actively with authorization from the patient.
Analysis of headache characteristics

The effects of headaches on activities at work, school and studies are particularly relevant for assessing the severity of the headache
The annual evaluation shows the aggregated data sets for the respective month of the year in Figure 3. The main headache phenotypes are differentiated in the first four columns. Column A contains the days with a migraine aura, column M the days with migraine, column S the days with tension-type headaches and column U for other types of headaches. Migraines and tension-type headaches account for over 92% of all headaches in the population. Therefore, the migraine app focuses on these two main forms. Since the International Headache Classification differentiates 367 main types of headaches, it is not possible to meaningfully document all headache phenotypes and headache subtypes [13,14].
Assessment of headache-related impairment
Using the migraine app requires a trained patient who can differentiate the type of headache they have in everyday life. Since the patient also needs to know in everyday life which type of headache he should use which acute therapy or other treatment measures, differentiating the headache phenotype is a prerequisite for professional treatment. Therefore, the digital care application does not need to prospectively query all features of the headache phenotype for each attack. The patient enters the relevant characteristics in the “Quick Entry” menu and also documents the severity, duration, type of acute medication used and its effectiveness. At the same time, he documents the effects of the headache on work activities, school or studies, on household activities as well as on social and leisure activities. The migraine app progressively records the degree of impact on these areas. A restriction of activity by more than 50% is documented to record the degree of impairment caused by headaches. The migraine app also records whether activity is completely impossible in the respective area due to headaches. If this affects work, school or study, a day of incapacity for work (AU) is registered. If household or leisure activities are made completely impossible, this will be documented as 100% impairment. The days of impairment caused by headaches are totaled per month and shown in the last column as GdBK points, as “degree of impairment due to headaches”. This means that the patient and doctor receive a direct quantitative image of the impairment caused by the headache in the respective month. This score is calculated analogously to the MIDAS score [15-17]. The MIDAS score records the corresponding impairments retrospectively from memory over a period of 3 months. It is evident that the value obtained in this way is much more prone to errors. In contrast to the MIDAS score, the data for determining the GdBK is continuously collected prospectively, so that the reliability is considered to be higher.
The direct analysis of the course parameters collected in this way can be used directly for the treatment decision. A significant decrease in the number of migraine days per month by at least 50% can operationally prove the effect of a chosen headache prophylaxis. The treating doctor can see directly whether, for example, the selected medication is effective or whether therapy needs to be adjusted by increasing the dose or changing the medication. By analyzing the number of headache days per month, the development of chronic migraines can also be mapped. If the sum of migraine days and days with other headaches is 15 or higher over a period of more than three months, the diagnosis of chronic migraine may be justified.

The migraine app contains, among other things, the simulation of a migraine aura. It shows what visual disturbances look like during migraine attacks. Since the symptoms of a migraine aura are often confused with those of a stroke, those affected and doctors can make a quicker and easier differential diagnosis
Analysis of the severity and duration of headache attacks
Whether the headache therapy is effective over time can also be determined by the severity and duration of the headache attacks. The sum of the individual values per month is calculated for the severity and duration and at the same time an average is calculated. The severity of the headache is documented with a score (0= none, 1= mild, 2= moderate, 3= severe, 4= very severe). The respective graduations are described in the legend on the evaluation PDF (see Figure 3). A reduction in the average severity and a reduction in the average duration of headache attacks can be used as an effectiveness of preventive treatment as well as acute treatment.
Analysis of drug effects
The operational assessment of the effect of acute therapy can be carried out by analyzing the effect of the medication. First, the days of intake for acute therapy are shown for each month. The decrease in the need for acute medication can also be interpreted as an indication of effective prophylaxis. On the other hand, the increase or even the increase in the number of days of intake per month to 10 or more days per month can be viewed as an indication of increasing chronicity and the development of a medication overuse headache. Here it is important to discuss in detail with the patient that the 10-20 rule must be adhered to and that exceeding the 10 limit promotes further chronicity. Simply by pointing out an appropriate limit on the amount of acute medication taken per month and possibly being instructed on how to take a medication break can significantly stabilize and improve the headache.
The effect of acute medication can be determined using the medication effect. For this purpose, a score for the medication effect is shown. The drug effect (grading 0= no effect, 1= weak, 2= medium, 3= good, 4= very good) shows an effect of 0 in the worst case and an effect of 4 in the best case. Ideally, a score between 3- 4, ie good to very good, is the aim. If the score is below 3, an adjustment of acute therapy should be considered.
Degree of headache impairment, GdBK score
The effects of headaches on activities at work, school and studies are particularly relevant for assessing the severity of the headache. This also applies to the impact on household activities as well as on leisure and social activities. The migraine app continuously and prospectively documents the degree of impairment caused by the headache for the respective areas and aggregates this data monthly. For each month, the sum of the affected areas of activity is created into an overall score. This overall score is referred to as the GDBK point score and quantitatively reflects the degree of impairment caused by headaches. The GDBK points can therefore directly quantify the headache-related impairments for the respective month. The increase or significant decrease can directly and quantitatively document the effectiveness of the headache treatment and the effects of the headache on the quality of life in the follow-up. A reduction in the GdBK score of 30% or more can be considered a clinically significant improvement.
The consultation checklist makes it possible for doctors and patients to immediately track headache symptoms over the last few months and to make individual, data-based therapy adjustments. However, it is essential that the doctor can make an appropriate interpretation of the data pattern. If the migraine app is trained accordingly, the migraine app is an objective tool for analyzing the course of the disease and optimizing therapy in care for both the patient and the doctor.
Table 1. Overview of the features and menu structure of the Migraine app
|
menu |
Features |
|
My overview (cockpit) |
Aggregated data analysis of the last 6 months Call up a checklist for the medical consultation to monitor progress and success Analysis of migraine and headache-related impairment |
|
Quick entry |
Entry of a new headache attack according to ICHD -3 criteria -Headache symptoms -Acute medication (retrieval from database, analysis 10-20 rule) -Headache-related impairment (GdBK) -Automatic supplementation of the weather data at the location -Comments on the attack |
|
Pain calendar |
Monthly presentation of the headache progression. Processing of the entered data |
|
Taking medication |
Documentation of preventative medications |
|
Evaluation |
Data aggregation for the doctor per month or |
|
More |
|
|
Aura simulation |
Simulation of a migraine aura in the |
|
Aura Demo Type 1 |
Rendering of a visual migraine aura with |
|
Aura Demo Type 1 |
Reproduction of a visual migraine aura with |
|
Chronification |
Scale for the analysis and prevention of |
|
Rapid test |
Rapid headache test to differentiate |
|
Triptan threshold |
Rapid test to determine the optimal time for taking acute medication (analgesics, triptans) |
|
Expert searches |
Locate and navigate to headache experts in the nationwide headache treatment network in the local area |
|
Progressive muscle relaxation |
Comprehensive audio instructions for training progressive muscle relaxation as a long form (45 minutes) |
|
Short progressive muscle relaxation |
Audio instructions for training progressive |
|
Muscle relaxation for children |
Audio instructions for training progressive |
|
information |
|
|
Pain Clinic Current |
Information center on current topics in migraine |
|
Media library |
Video library on current topics in migraine |
|
Headache knowledge |
Library on current topics in migraine |
|
Headache classification |
Original version of the International |
|
Communities |
|
|
Headbook Community |
Digital self-help group for migraines and |
|
Live chat |
Expert live chat on questions about migraine |
|
Facebook community |
Digital exchange on migraines and |
|
Settings |
|
|
Memories of PMR |
Memories of |
|
Warning 10-20 rule |
Warning if acute medication intake is exceeded |
|
Memories preventive medication |
Reminder function for preventive medication to be taken daily, every 4 weeks or 3 months |
|
MIDAS score |
Retrospective analysis of migraine-related disability using MIDAS score |
|
Backup/Export |
Data protection via backup, export and transfer to another device (only possible actively by the user) |
|
Video instructions |
|
|
Video clips |
Video clips explaining the different functions of the migraine app |
literature
- Diener HC, Gaul C, Jensen R, Göbel H, Heinze A, Silberstein SD (2011) Integrated headache care. Cephalalgia 31(9):1039–1047. doi:10.1177/0333102411409075
- Göbel H, Heinze A, Heinze-Kuhn K, Henkel K, Roth A, Ruschmann HH (2009) [Development and implementation of integrated health care in pain medicine: the nationwide German headache treatment network]. Pain 23(6):653–670. doi:10.1007/s00482-009-0857-7
- Göbel H, Heinze-Kuhn K, Petersen I, Göbel A, Heinze A (2013) [Integrated headache care network. Kiel Migraine and Headache Center and German National Headache Treatment Network]. Pain 27(2):149-165. doi:10.1007/s00482-013-1307-0
- Göbel H, Frank B, Heinze A, Zimmermann W, Göbel C, Göbel A, Brunkhorst J, Rupp K (2019) Health behavior of migraine and headache patients during digital therapy support with the migraine app. The Pain 33 (2):147-155. doi:10.1007/s00482-018-0355-x
- Diener HC, Brune K, Gerber WD, Göbel H, Pfaffenrath V (1997) Treatment of migraine attacks and migraine prophylaxis. Dtsch Ärztebl 94 (46)
- Wallace LS, Dhingra LK (2014) A systematic review of smartphone applications for chronic pain available for download in the United States. J Opioid Manag 10(1):63–68. doi:10.5055/jom.2014.0193
- Martinez-Perez B, de la Torre-Diez I, Lopez-Coronado M (2013) Mobile health applications for the most prevalent conditions by the World Health Organization: review and analysis. J Med Internet Res 15(6):e120. doi:10.2196/jmir.2600
- Rosser BA, Eccleston C (2011) Smartphone applications for pain management. J Telemed Telecare 17(6):308–312. doi:10.1258/jtt.2011.101102
- Hundert AS, Huguet A, McGrath PJ, Stinson JN, Wheaton M (2014) Commercially available mobile phone headache diary apps: a systematic review. JMIR Mhealth Uhealth 2(3):e36. doi:10.2196/mhealth.3452
- Oltrogge JH, Brockmann S, Scherer M (2018) Headache in general practice. Journal of General Medicine 7-8:306-312
- Jamison RN, Raymond SA, Levine JG, Slawsby EA, Nedeljkovic SS, Katz NP (2001) Electronic diaries for monitoring chronic pain: 1-year validation study. Pain 91(3):277-285
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR (2003) Patient compliance with paper and electronic diaries. Control Clin Trials 24(2):182-199
- IHS (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1-211. doi:10.1177/0333102417738202
- Olesen J (2018) International Classification of Headache Disorders. Lancet Neurol 17(5):396-397. doi:10.1016/S1474-4422(18)30085-1
- Stewart WF, Lipton RB, Kolodner K (2003) Migraine disability assessment (MIDAS) score: relation to headache frequency, pain intensity, and headache symptoms. Headache 43(3):258–265
- Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN (2000) Validity of the Migraine Disability Assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain 88(1):41-52
- Stewart WF, Lipton RB, Whyte J, Dowson A, Kolodner K, Liberman JN, Sawyer J (1999) An international study to assess reliability of the Migraine Disability Assessment (MIDAS) score. Neurology 53(5):988-994







Leave a comment