The first week of September is used internationally to educate people about migraines in order to raise awareness of the great importance of the health problem. Prejudices and stigmas should be reduced. Prof. Hartmut Göbel answers current questions about migraines, their effects and treatment:
How important are migraines and headaches to society?
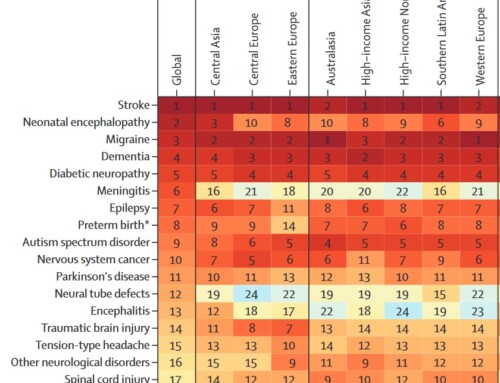
Representative studies show that 71% of Germans say they will suffer from headaches in their lifetime. The number includes all 367 different types of headaches known today. There are around 54 million people living in Germany who constantly have to endure headaches. Headaches can occur over long periods of life, often over 40-60 years. They lead to great suffering and significant restrictions on quality of life and ability to work. The World Health Organization lists migraine as the 7th most severely disabling disease. If you take all headaches together, headaches are the third most severely disabling illness in humans.
Migraines have always existed as long as humans have existed. A first severe migraine attack is described in great detail on an Egyptian papyrus. Migraine attacks are repeatedly documented in world literature. The Apostle Paul's Damascus experience with light phenomena and three days of lying down with loss of appetite also prove that migraines are not a modern phenomenon, but have existed since time immemorial.
And here are some important facts:
- Migraine is the third most common disorder in the world (behind dental caries and tension-type headaches) with an estimated global one-year prevalence of 14.7% (i.e., approximately one in seven people). Almost every third woman between the ages of 30 and 40 is affected.
- Migraines are more common than diabetes, epilepsy and asthma combined.
- Chronic migraine affects approximately 2% of the world's population.
- Migraines affect three times as many women as men.
- 900,000 people in Germany are affected every day. 100,000 people are unable to work and bedridden every day because of migraines.
- On average, 8.3 million Germans take a headache tablet every day through self-medication.
- On average, 58,853 individual doses of triptan, which are special migraine medications for treating migraines, are taken every day in Germany
- More than half of those affected experience severe impairment as a result of the attacks.
- Migraines often begin during puberty. It is most disabling between the ages of 35 and 45. But many young children are also affected. In recent years there has been a strong increase, particularly among children.
- Migraine is the seventh most debilitating disease worldwide and the leading cause of disability among all neurological diseases.
- It is estimated that the German population loses 32 million working days due to migraines.
- Severe migraine attacks are classified by the World Health Organization as one of the most disabling diseases, comparable to dementia, paraplegia, which affects all four limbs - both legs and arms - and active psychosis.
- Migraines and chronic headaches are the second most common reason for short-term incapacity to work.
- Incapacity to work due to migraines alone costs 3.1 billion euros per year in Germany, calculated based on 32 million days lost.
- The risk of depression, anxiety disorders and suicide is 3 to 7 times higher in those affected than in healthy people.
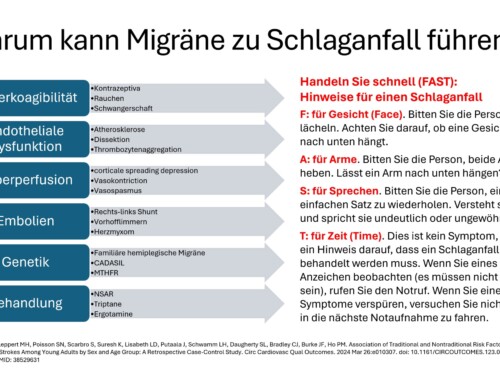
- The risk of circulatory diseases, heart attack and stroke is 1.5 to 2 times higher than in healthy people. This is particularly true for young women under 45 years of age.
- It is scientifically proven that migraines have a genetic basis. 44 gene variants for 38 risk genes for migraine are now known.
- One of the most common health problems treated with scientifically unsupported unconventional therapies is headache.
- Worldwide, on average only about two to four hours of information about headache diagnosis and treatment are offered during the six-year medical course.
- Despite the proven effectiveness of the use of specialist nurses for headache treatment, there is currently no specialized training in Germany.
- Migraine and other headaches were first classified internationally in 1988 by the International Headache Society (IHS) and operationalized diagnostic criteria were described. The International Classification of Headache Disorders, 3rd Edition (ICHD-3) beta was published in 2013 and is recognized by the World Health Organization. Researchers and clinicians worldwide refer to these internationally valid diagnostic criteria. Today there are 367 main diagnoses of headaches. No other neurological disease has a comparable, differentiated diagnosis and classification system.
Migraines are sometimes still seen as an excuse?
Unfortunately, complete ignorance or, at worst, ill will must be assumed here. The fact that people are discriminated against because of a disability or genetic makeup should be a thing of the past. Migraine is a biological human disease. The World Health Organization lists it as one of the most severely disabling human diseases. Today, 44 gene variants have been decoded into 38 risk genes, which prove that biological conditions in our body's blueprint are responsible for the risk of migraine disease. Migraine is a serious disease of the nervous system that causes severe individual suffering and severely disables those affected.
Should there be more information about migraines and headaches?
Many people who suffer from headaches do not have a specific diagnosis. Only about a third have a name for the headache. Today, over 367 headaches are distinguished internationally. Most of them are not even known by name in average medical care. Special treatment concepts are not available to those affected. Patients themselves also have no concept, no idea where the headaches come from or how they should be specifically treated. It is therefore of the utmost importance that those affected are given specific treatment options.
How do you recognize migraines and tension headaches?
Migraine attacks are episodic headaches that last 4-72 hours. The headache has a pulsating, throbbing character. It can be felt in a specific area of the head. Physical activity increases the pain, the pain has a very strong intensity, which is why the activity is severely hindered or made completely impossible. The pain can be accompanied by nausea, vomiting and hypersensitivity to noise and light. The tension-type headache, on the other hand, occurs as a dull, pressing, bilateral headache. Physical activity does not increase the pain, and nausea and vomiting are not present.
Are women affected more often?
According to representative studies, women suffer from migraines about 2 to 3 times more often. Scientific studies indicate that faster, more active processing of stimuli in the central nervous system is responsible for this.
Why do some people get migraines and others don't?
The latest research has shown that specific risk genes increase the likelihood of developing migraines. In the world's largest migraine study to date, 44 new gene variants were discovered. They are associated with an increased risk of developing migraines. Many of these gene variants are located in the areas of the genome that regulate the brain's circulatory system. The new discoveries indicate that a disruption in the blood and energy supply to the brain is essential for the development of migraines. They are a milestone in understanding the causes of migraines.
How does migraine behave over the lifespan?
As a rule, the first attacks occur in the 7th year of life. From the age of 14, more than 14% of girls and more than 7% of boys are affected. The peak frequency of migraines is in the third and fourth decades of life.
Which doctor should I contact if I have migraines and headaches?
Migraine is a neurological disease of the central nervous system. If left untreated, it can lead to serious complications. In addition to psychological complications, serious physical illnesses can also occur if a migraine is not treated effectively. These include an increased risk of stroke, heart attack and other cardiovascular diseases. There are still some people who believe that this serious illness should be treated with unconventional or alternative therapeutic methods. There is definitely no room for this based on current scientific knowledge. Migraines must be treated as effectively as possible so that they do not become chronic and serious long-term complications are avoided. The first point of contact is the general practitioner. If the course of the disease is complex, the neurologist is called in as a specialist; for severe illnesses, the pain therapist is also the special contact person.
What happens in the brain?
Basically, with migraines there is no structural disorder in the brain, so the structure of the brain is normal. However, due to their genetic makeup, migraine patients can differentiate stimuli very quickly and very effectively; anything too fast, anything too many, anything too sudden, anything that hits the nervous system at once will lead to strong activation of the nerve cells, with the result that Energy reserves in the nerve cells are exhausted. This repeatedly leads to a derailment of the regulation of the nerve function, it can collapse and a migraine attack can occur.
If such a miscontrol of nerve function occurs, inflammatory substances can be released in the arteries of the meninges. These lead to increased sensitivity of the meninges. Every pulse beat leads to a throbbing, pounding migraine pain, every movement of the skull hurts. That's why migraine sufferers try to rest as much as possible and avoid physical activity. Migraine pain is therefore based on neurogenic inflammation with increased pain sensitivity.
What triggers seizures?
The most important factor that triggers migraine attacks is irregularity in everyday life and excessive energy demands on the nerve cells. Stress, irregularity, everything too fast, everything too much, everything too sudden, all at once, can trigger migraine attacks.
How do you treat migraines today?
Contemporary migraine therapy is based on three crucial pillars. The first pillar consists of knowledge and information. Migraine sufferers need to know how migraine attacks occur, what happens in the nervous system and how they are triggered. You need comprehensive information about behavior and measures to protect yourself from migraines. This primarily includes a regular day-night rhythm. Patients should eat regular meals. Meals rich in carbohydrates are recommended because the nervous system depends on carbohydrates. Migraine attacks occur due to an energy deficit in the nerve cells, due to the high activity, which is genetically determined. Sufficient drinking, regular sleep and regular breaks in everyday life should also be initiated. Learning relaxation training such as progressive muscle relaxation can significantly reduce the frequency of migraines. Information from a patient guide or through information on the Internet can also provide a lot of knowledge that helps reduce the frequency of migraines in everyday life. Self-help groups such as B. the internet platform www.headbook.me can lead to exchange and pass on knowledge to those affected. Sports therapy is also well suited to reducing the frequency of migraine attacks. Regular endurance sports such as running, swimming or cycling are particularly helpful. If you have more than seven headache days per month, medication prophylaxis should be considered in addition to the measures described. This consists of different medication options and includes the administration of beta blockers, calcium antagonists, antiepileptics, antidepressants and other substances. An individual selection should be made; this must be discussed with a doctor. There are various options for treating the acute attack. For mild attacks, painkillers such as aspirin, ibuprofen or paracetamol can be used; for nausea and vomiting, this is combined with the administration of so-called anti-nausea and vomiting agents such as: B. Metoclopramide. For severe attacks, seven different triptans are available in different dosage forms. In the event of severe nausea or vomiting, the active ingredient can also be injected under the skin using a pen; it is also available as a nasal spray. Triptans should be taken as early as possible in the attack and the 10-20 rule applies here too. They should be used less than 10 days per month to avoid medication overuse headache (MHD). New treatment options for chronic migraines, ie migraines that occur more often than 14 days a month, are botulinum toxin and neuromodulation. These can be used by specialized headache centers in particularly severe cases.
What mistakes can you make?
The most common mistake is that information on behavior, prevention, etc. is not implemented. Many attacks will then occur very quickly, which means that acute medication will be taken too often. If you take acute medication for at least ten days or more, the sensitivity in your nervous system changes. The result is increased sensitization with the development of a headache when medication is overused. A cycle of more and more attacks then ensues, with the need to take acute medication more and more frequently until a permanent headache develops. Therefore the most important rule: acute headache medication should be taken on fewer than 10 days per month. Acute medications should not be used to treat headache attacks for at least 20 days per month.
Do you have to put up with migraines?
You can't put up with pain and migraines. You don't get used to pain. On the contrary: pain causes even more pain. Enduring pain is not a virtue. You have to actively treat them. With today's therapy options, there are very effective and sustainably tolerated therapy strategies to deal with headaches. However, you have to become your own advocate, take initiative, obtain knowledge and information in order to then implement targeted preventive measures.
How do you proceed with treatment at the Kiel Pain Clinic?
Our treatment concept focuses on neurological pain disorders such as migraines, chronic headaches and other pain disorders associated with diseases of the nervous system. These are among the most disabling conditions and, after dementia and stroke, one of the three most expensive neurological diseases. Traditional sectoral care and medical specialist boundaries increase their tendency to become chronic. The core is multimodal pain therapy, ie the consistent interdisciplinary implementation of international scientific knowledge to the needs of patients, indication-specific cooperation between specialized practitioners and networking. The aim is to provide lasting pain relief, rebuild quality of life and restore the ability to work. The clinic has received multiple awards for its innovative treatment concept, including the prize for the best implementation of integrated care in Germany. Patient satisfaction in the nationwide treatment network is very high. This is confirmed to us again and again by patients and also the health insurance companies.
What advice do you give relatives?
Relatives of migraine patients should also find out more about the development and maintenance of migraines. They can then understand their family members, show them understanding and support them in implementing preventive measures. Reading a patient advice book and getting involved in self-help groups can provide significant support. Social communities on the Internet such as www.headbook.me
What's the future like?
Migraines are being researched very intensively internationally. It has become better understood in recent years that migraine is a very severe, serious neurological disease. You may not die from it acutely, but the pain, disabilities and complications can still cost your life. The enormous social impact of migraines must also be reduced. Therefore, there are new research strategies and efforts in many fields. They lead to a better understanding of the causes of migraines. New therapeutic methods are also on the horizon. Current research is aimed, among other things, at monoclonal antibodies, immunologically active proteins that stop the inflammation in migraines. The so-called CGRP, an inflammatory protein, plays a central role. Antibodies against it are currently being developed and tested in numerous studies. If the results are positive, the antibodies could be used in the future as a kind of passive vaccination against migraines.






Leave a comment