Almost 15 percent of Germans suffer from migraines. Professor Hartmut Göbel says what patients should pay attention to and what can help them. The research gives hope. Migraines are one of the diseases that most commonly affect people in Germany. One person who knows this particularly well is Professor Hartmut Göbel. He is the founder, medical director and managing director of the pain clinic in Kiel. The holder of the Federal Cross of Merit also launched a course on migraines at the University of Kiel. In an interview with editor Matthias Jansen, Göbel talks about the disease, who it affects, what can be done about it and what research is currently working on.
Are the numbers correct that up to 15 percent of Germans suffer from migraines?
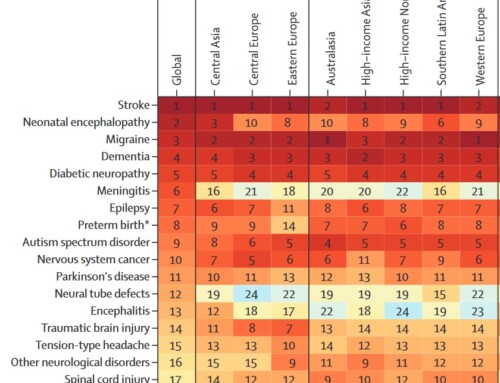
Within a year the number is correct. The frequency must always be related to a period of time. If you look at the entire life, around 40 percent of the population suffers from migraine attacks. After tooth decay and tension-type headaches, migraines are the third most common human illness. It is also the reason for the most severe disability among people under the age of 50.
Are headaches increasing in our fast-paced world?
In fact, studies show that headaches have become significantly more common in recent decades. This particularly applies to children and young people. Headaches have always been a very big problem in adults too. Primary headaches, migraines and tension headaches are the most common neurological diseases. While many patients previously gave up and hoped for alternative medical treatments, many of these affected people are now specifically diagnosed and can be offered successful therapy in the medical field. However, stress, irregularities in everyday life and family pressures can also worsen headaches. In this respect, current psychosocial factors are also an aspect of the greater frequency and severity of headaches in our time.
Is it true that more and more children are affected? How does this happen and how can they be helped?
Studies over the last few decades show that headaches in children have increased significantly. Long-term studies show that there is an increase of more than 300 percent in the frequency of headaches, especially in young children. Children today live in an unstable world, and families' frequent moves play a role. The workload on parents can also have a negative impact on headaches in children. Consuming media, especially digital applications, can also put a strain on a child's nervous system and make headaches more frequent. Maintaining a consistent rhythm and a regular daily routine are particularly important for children. Times for relaxation and balance should be allowed. A regular, carbohydrate-rich diet is an important prerequisite for sufficient energy supply in the nervous system. A regular sleep rhythm should also be observed. A precise diagnosis and an effective therapy concept are particularly important for children so that headaches do not become chronic and become more frequent at a young age.
When do headaches become chronic?
If a headache occurs on more than 15 days a month for more than three months, it is called a chronic headache. It is therefore particularly important that the frequency of headaches is reduced through treatment. The more frequently headaches occur and the more headache days there are per month, the more difficult the treatment is and the greater the effort required to implement effective therapy.
Who is most affected by the disease and why do people get migraines?
It particularly affects women because they have a more active, faster nervous system. You can absorb and process stimuli and emotions more intensively. This is the background why the female nervous system requires a greater energy turnover and therefore energy deficits are more pronounced. In addition, there are greater changes in metabolism and energy supply as part of the menstrual cycle. Migraines are therefore not an age-related disease. Migraines require an active reactive brain. Migraine sufferers are able to think very quickly and very actively. This high level of nervous activity requires a high energy turnover in the nerve cells. However, if there is an energy deficit, this means that the nerve cells cannot work adequately at times. Nerve function is disrupted or breaks down. The typical consequences of a migraine attack then arise.
What are the consequences?
Some patients experience neurological deficits such as zigzag lines with flickering vision in front of the eyes, speech disorders, dizziness, tingling sensations or even paralysis. Then comes the headache. The pain lasts between four and 72 hours. The pain can occur on one side. The character of the pain is pulsating and throbbing. Physical activity can increase pain, requiring patients to remain in bed. Nausea, vomiting and hypersensitivity to noise and light can accompany the pain.
Why is migraine not really present as a disease?
Migraine sufferers usually suffer alone. You live behind drawn curtains, you're grounded for three days, you don't eat or drink anymore, the environment doesn't notice you, you're out of work. Migraine is the forgotten epidemic. Although so many people are seriously ill with it throughout their lives, overall awareness of the importance of migraine is still low. Fortunately, there has been a significant improvement in recent years. The need for society to advocate for this group has only become increasingly recognized in recent years.
How do you go about trying to diagnose migraines?
Headache diagnosis consists of several steps. First, the exact picture of the headache process must be recorded and analyzed. Since there are now over 367 main types of headaches, this is a very complex and time-consuming process. The affected patients have to describe very precisely how the headache occurs. Headache questionnaires, headache calendars and the migraine app can provide very valuable help. People can also experience multiple types of headaches at the same time or at different times. Therefore, all these different types must be delineated and differentiated.
What happens then?
The next step is to carry out a very careful neurological and general medical examination. When taken together, most patients show symptoms of a so-called primary form of headache. This means that the headache is the actual illness and not a symptom of anything else.
And if not?
However, if doubts arise, these must be substantiated or ruled out and further targeted diagnostic measures must be taken. The conditions for the headache to occur must be addressed therapeutically. For example, a headache caused by high blood pressure cannot be effectively treated with a painkiller. The high blood pressure must be treated. As a result, the headaches subside.
Is it true that migraines start during puberty?
Migraines often begin when you start school. It is the period when the brain is mature enough to learn and act quickly. Migraines typically start more frequently in boys. However, the girls then quickly overtake them and from puberty onwards, boys outnumber girls 1:3.
Those affected say that the only thing that helps with migraines is taking medication. What is to be considered?
With 367 main types of headaches, it is understandable that there are very different ways to treat headaches. Every headache treatment should begin with information and education about the diagnosis and the concept of the disease. This is then followed by behavioral measures to treat headaches through lifestyle, diet, relaxation, exercise or regulating your daily routine. The next step for headaches that occur in attacks is to clarify the attack therapy. Painkillers also play an important role in the treatment of headache attacks. Specific prevention of headaches is particularly important. This is due to the fact that the administration of triptans or painkillers alone is not sufficient to effectively treat headache disorders. This is especially true if the headaches occur very frequently. If you take acute medication for migraines on ten or more days a month, a so-called medication overuse headache can occur. This means that headaches become more frequent, they respond less well to acute medication and eventually a permanent headache can develop. It is therefore of great importance that effective prevention of headaches is found. The aim is to reduce the frequency of headaches and, if possible, to make the frequency of headaches as low as possible.
You mentioned the behavioral measures. What can migraine sufferers do to feel well without medication?
Modern pain therapy does not differentiate between either or. Rather, everything that has proven to be effective in scientific studies should be made available to the patient. Nutrition, sports therapy, relaxation, knowledge, information and other non-drug procedures are essential components of modern and effective pain therapy. The nervous system needs complex carbohydrates for healthy activity. Due to genetic factors, the nerve cells of migraine sufferers are particularly active. During a migraine attack, there is an increased consumption of energy. As a result, an energy deficit occurs. The nerve cells can no longer work adequately and a migraine attack occurs.
How can patients contribute through their diet?
It is important that those affected consume enough complex carbohydrates, such as potatoes, rice or whole grain products. A regular eating rhythm should be maintained. The feeding intervals should be maintained consistently. Omega-3 fatty acids have also been proven in scientific studies to be effective as a preventive measure. They reduce inflammatory processes in the nervous system. Therefore, care should be taken in the diet to ensure that sufficient omega-3 fatty acids are consumed. Relaxation techniques, biofeedback and sports therapy have proven particularly useful for behavioral prevention. Behavioral therapy measures can also be effective for severely affected patients.
Is migraine a hindrance to pursuing a professional career?
In fact, people with migraines are particularly productive. You have a very active, creative brain. Their genetic makeup means they can implement innovative ideas, quickly perceive problems and find solutions. In addition, migraine sufferers often suffer their attacks after an active phase, which is typically Saturday and Sunday. On Monday they will be there again and can once again contribute their skills to society. Smart employers therefore best hire migraine sufferers. In many areas there are well-known migraine sufferers who do excellent work. From this point of view, the idea that migraine makes you less productive is completely inadequate and does not correspond to the current state of science.
Which patients come to your clinic?
Severely affected patients with chronic pain disorders are admitted to the Kiel Pain Clinic nationwide. A special feature is that despite numerous attempts at therapy, these could not be treated effectively. Pain leads to a high level of suffering and the quality of life is severely impaired. Many patients can no longer work or are at risk of early retirement. Due to persistent pain or a high frequency of attacks, medication must be taken very frequently. Overuse of medication can occur, with the result that pain paradoxically becomes even more frequent. The pain medications are less effective. At the same time, the pain increases in frequency and intensity. The severe impairment of pain leads to anxiety, loss of confidence, hopelessness, depressive thoughts, social withdrawal, sleep disturbances and complex psychosocial effects. In addition, many patients also suffer from complicated physical comorbidities. These make pain therapy more difficult. For example, diseases of the stomach, intestines and liver can prevent you from taking certain medications. Overall, it is not an isolated symptom of “pain”, but rather a complex illness with a wide range of effects.
At what point should I get help for a headache?
Headaches can be very complex illnesses and should be diagnosed by a doctor. If other types of headache occur that are not yet known, headaches become more frequent, lead to severe suffering and hinder professional, social and family life, and medical treatment should be sought. The same applies to headaches, in which unclear physical symptoms occur as an accompanying problem. Examples include fever, chills, neck stiffness, joint pain, muscle pain, increasing neurological and psychological symptoms.
What has changed in the treatment of different types of headaches in recent years? What is being researched?
In recent years, a significant improvement in migraine prevention has been achieved through the introduction of antibodies against CGRP, the calcitonin gene-related peptide. CGRP is an important messenger substance that plays a central role in migraines. It causes the veins of the meninges to expand and become inflammatory. The result is a pulsating, throbbing and pounding headache. Through decades of research, it has now been possible to develop specific substances that inhibit the effect of CGRP on migraines. Four so-called monoclonal antibodies are approved for treatment. They demonstrate high effectiveness in practical use. In addition, they are generally well tolerated. They also work in patients who do not respond to current medications approved for migraine prevention. Other substances such as Ditane or Gepante are in development for attack therapy; they have already been approved or are about to become available.
What exactly is immunotherapy to prevent migraines?
During a migraine attack, the neurotransmitter CGRP is increased. With effective treatment with a triptan it can be reduced. This substance is generally increased in patients with chronic migraines. Giving CGRP to migraine patients can also trigger a migraine attack. The antibodies developed in recent years either block the substance itself or the CGRP receptor. The medication is given to the patient using an auto-injector or as an infusion at intervals of four weeks or three months. They do not lead to permanent immunity, but have to be used again and again to stop the messenger substance. One can therefore speak of a so-called passive immunization or immunotherapy against migraines. Treatment with monoclonal antibodies has significantly improved migraine therapy. Patients who previously could not be helped can experience a significant reduction in their migraine attacks and a completely new quality of life. However, not all patients respond to this therapy. Drug treatment should never be the sole component of contemporary migraine therapy.
And is there an active vaccine against migraines on the horizon?
Monoclonal antibodies against CGRP have been shown to be effective in preventing migraines as passive immunotherapy. In fact, we are currently working on a vaccine that will stimulate the body's active production of antibodies against CGRP. This could provide another new option for preventing migraines in the future. Immunogenicity studies with the active ingredient UB-313 have so far been carried out experimentally. Vaccine-induced endogenous serum antibodies were characterized for their binding and functional properties. Initial studies show that immunization with UB-313 actively elicits anti-CGRP antibodies. These antibodies can bind human CGRP and exhibit dose-dependent functional inhibition of CGRP. This suggests antibody properties comparable to those of already approved monoclonal antibodies. The vaccine UB-313 has been in clinical development since September 2022: The ongoing phase 1 study is intended to investigate safety, immunogenicity and target effect. As a potentially safe and effective immunotherapy against CGRP, UB-313 may represent a cost-effective and practical strategy for migraine prevention.







Leave a comment