The diseases headache and migraine not only affect the lives of those affected, but also cause economic damage. Newly developed antibodies specifically intervene in the molecular development process of migraines and can therefore preventively reduce the likelihood of migraine attacks.
By Hartmut Göbel
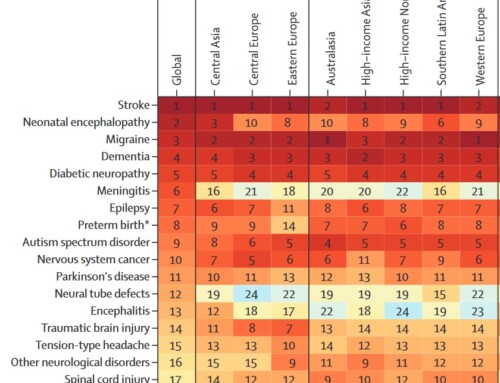
Every day, around 900,000 people in Germany alone suffer from migraine attacks, and 100,000 people are unable to work and are bedridden every day due to migraine attacks. This makes migraine the third most common disease in humans worldwide behind tooth decay and headaches; migraine is the most important reason for disability in people under 50. On average, three million Germans take a headache tablet every day through self-medication. In addition, almost 60,000 individual doses of triptan, special acute migraine medications, are used nationwide every day to treat migraine attacks. The disease also has an impact on the economy: headaches are one of the most common reasons for short-term inability to work. The number of days missed per year due to migraine throughout Germany alone corresponds to the annual working hours of 185,000 full-time employees - with an estimated cost of 3.5 billion euros. In addition, there is the loss of productivity due to unpaid work in the household, in raising children or in caring for relatives. The risk of cardiovascular disease, heart attack and stroke is 1.5 to two times higher than in healthy people; the risk of developing depression, suffering from an anxiety disorder or committing suicide is even three to seven times higher in migraine patients. The total annual cost of headaches in 18 to 65 year olds in Europe is over 170 billion euros. And across Europe, less than twenty percent of those affected receive medical care, and less than ten percent receive prevention or acute therapy in accordance with guidelines.
Gene variants increase the risk of disease
Now, new study results have shown that migraine patients have numerous peculiarities in their genetic makeup. There are now 38 gene loci with 44 gene variants known that increase the risk of getting migraines. These gene variants are responsible for stimulus transmission, stimulus sensitivity and stimulus processing. In addition, they control the regulation of the energy supply to nerve cells and artery walls. These coverings of the veins are the largest endocrine organ in which numerous messenger substances are produced that control blood circulation but also regulate inflammatory reactions. Many substances are also activated here that are relevant for important control processes in the body. A disruption in the energy supply, for example due to oxidative stress, can throw this regulation out of balance and trigger malfunctions. Hereditary factors as well as environmental, behavioral and social factors play a significant role in the development of migraine attacks. If the nerve function is miscontrolled, inflammatory substances can be released in the arteries of the meninges, which lead to increased sensitivity of the meninges. Every pulse beat causes a throbbing, throbbing pain, every movement of the skull hurts. That's why migraine sufferers try to lie down if possible, limit physical activities and avoid vibrations.
Antibodies can reduce migraine attacks
In recent years, it has been possible to develop specific antibodies against messenger substances that trigger inflammation during a migraine attack. The focus is on the Calcitonin Gene-Related Peptide, or CGRP for short, which is one of the strongest vasodilators and plays an important role in the development of migraines. If the patient receives so-called monoclonal antibodies, the effects of these inflammatory substances can be stopped for a few weeks, thereby reducing the likelihood of migraine attacks. The antibodies erenumab, galcanezumab, fremanezumab and eptinezumab have now been developed, which act directly against CGRP or block the receptor for CGRP. The four active ingredients have been tested in numerous large-scale, international studies and their effectiveness has been proven. There are study data for episodic migraine with up to 14 migraine days per month and for the chronic form with more than 15 migraine days per month. Among other things, it was examined whether the new antibodies also work in patients who did not respond to previously approved preventive medications. However, there are still no comparative studies with previous preventive medications. The annual therapy costs will probably be between 6,000 and 10,000 euros, but it is currently not clear for which types of migraine and for which patients the costs will be reimbursed by the health insurance companies. In order to meet the cost-effectiveness requirement, the new immunotherapy will certainly only be considered if the currently available migraine medications are not effective for a patient, are not tolerated or cannot be taken due to contraindications. Erenumab was the first of the four antibodies to be approved in Germany in July and will be available in pharmacies from November this year.
Immunotherapy specifically for migraine prevention
The antibody is injected every four weeks using an autoinjector, similar to an insulin pen. Since this immunotherapy is a passive immunization in which the antibodies are not produced in the body itself but are produced in the laboratory, the injection must be repeated regularly. In contrast to all other previously available medications that are taken for prevention, the new therapy has been developed specifically for migraine prophylaxis for the first time. A slow dosage increase due to intolerances and side effects is not necessary. The effect occurs within a few days; with the preventative medications currently available, the effect is often only achieved after weeks or even months. Side effects such as weight gain, mood changes, tiredness, reduced drive or drowsiness do not occur. In contrast to previous medications, which are often discontinued after a short time due to these side effects, the treated patients stick with this therapeutic principle for the long term due to its good tolerability and effectiveness. However, the data available so far show that the new immunotherapy does not stop migraines, but rather only reduces the risk of attacks: On average, headaches are reduced by around one to three days per month. This means that the effectiveness of the new vaccination is similar to that of previously available medications that are taken as a preventive measure. However, the advantages outweigh the advantages: the effect occurs quickly, the medication is well tolerated and even patients who have not been helped by other treatments respond to the therapy. Therefore, in the future, many more patients can certainly be helped to reduce the stressful migraine attacks in order to return to a relatively normal life.
Professor Dr. med. Dipl.-Psych. Hartmut Göbel , specialist in neurology, is the founder and director of the pain clinic and the migraine and headache center in Kiel. He is also the initiator and head of the nationwide headache treatment network.
Article in the Frankfurter Allgemeine Zeitung from October 26, 2018








Leave a comment