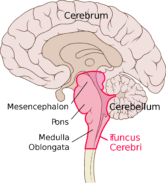
NDR Visite – Abenteuer Diagnose reports on a patient with years of unclear and complex neurological symptoms, including headaches. Among the 47 different subtypes of migraine, migraine with brainstem aura is often difficult to distinguish from other illnesses. So-called brainstem symptoms such as dizziness (vertigo), ringing in the ears (tinnitus), bilateral sensory and motor disturbances, as well as the inability to speak (dysarthria), swallow (dysphagia), and see double (diplopia) can occur. These symptoms can sometimes be difficult to differentiate from transient ischemic attacks (TIAs) or strokes.
Brainstem symptoms such as dizziness, tinnitus, bilateral sensory and motor disturbances, as well as dysarthria, dysphagia, and diplopia are not easily recognized in everyday life migraine with brainstem aura , and this form can sometimes be difficult to distinguish from transient ischemic attacks (TIAs). However, the following factors help in differentiating the two: patients with migraine with brainstem aura are generally in their second or third decade of life , vascular risk factors are absent , the headache in migraine with brainstem aura is severe , and the headache persists for a considerable time beyond the neurological symptoms .
If the basilar artery's territory is affected, bilateral motor disturbances can occur. Additionally, visual disturbances may be present in both the temporal and basal visual fields of both eyes, as well as dysarthria, dizziness, tinnitus, hearing loss, double vision, ataxia, bilateral sensory disturbances in the form of paresthesia, loss of consciousness, and even coma. In isolated cases, further symptoms have been described, such as cerebellar dysfunction, tremor, nystagmus, retinal degeneration, deafness, and ataxia.
In addition to visual aura, migraine with brainstem aura is also a common manifestation of migraine aura in childhood . Children with migraine aura may experience neurological disturbances such as bilateral visual field defects, loss of muscle tone, nystagmus, double vision, dysarthria, and altered consciousness . While attacks typically occur at long intervals, they can last from 24 to 72 hours. Given these accompanying neurological symptoms, a thorough examination by a neurologist essential in childhood.
The following are of particular the differential diagnosis : a tumor in the posterior fossa , drug side effects (e.g. antiemetics), mitochondrial disorders and metabolic diseases .
Details on the distinction between migraine and transient ischemic attacks (TIA) can be found here:
diagnostic criteria apply to migraine with brainstem aura :
Previously used terms
Basilar artery migraine; basilar migraine; migraine of the basilar type.
Description:
A migraine in which the aura symptoms are clearly attributable to the brainstem and there is no motor weakness.
Diagnostic criteria:
- Attacks that meet the criteria for a 1.2 migraine with aura and criterion B below
- Auras where both of the following points are fulfilled:
- At least 2 of the following fully reversible brainstem symptoms:
- Dysarthria1
- dizziness2
- Tinnitus
- Hearing loss3
- Double vision4
- Ataxia not attributable to a sensory deficit
- Impaired consciousness (GCS ≤13)5
- No motor or retinal symptoms.
- At least 2 of the following fully reversible brainstem symptoms:
Note:
- A distinction should be made between dysarthria and aphasia.
- Dizziness does not include lightheadedness and must be distinguished from it.
- This criterion is not met if patients report a "feeling of fullness" in the ear.
- Diplopia does not include (or excludes) blurred vision.
- An assessment of the level of consciousness according to the Glasgow Coma Scale (GCS) may have already been carried out upon admission; alternatively, deficits clearly described by the patient allow for a GCS classification.
- If motor symptoms are present, the condition is coded under 1.2.3 hemiplegic migraine.
Comment:
Originally, the terms basilar artery migraine or basilar migraine were used, but since involvement of the basilar artery is unlikely, the term migraine with brainstem aura should be preferred.
During most attacks, typical aura symptoms occur in addition to the brainstem symptoms. Many patients who experience attacks with brainstem aura also report other attacks with typical aura. In these cases, both 1.2.1 Migraine with typical aura and 1.2.2 Migraine with brainstem aura should be coded.
Many of the symptoms listed under criterion B1 can be misinterpreted, as they can also occur in conjunction with anxiety and hyperventilation.
Genetic predisposition with specific risk factors increases an individual's susceptibility to migraine attacks. The attack itself is characterized by an episodic dysfunction of the brainstem in the region of the trigeminothalamic projections. The trigeminocervical complex is activated and modulates nociceptive input from the extracerebral intracranial vessels and the dura mater. Muscular hyperpathia and allodynia, as well as central sensitization, arise via projections of the upper cervical nerves (C1, C2) to the spinal trigeminal nucleus. The release of neuroinflammatory neuropeptides and the activation of neurotransmitters in the extracerebral intracranial vessels and the dura mater result in vascular hyperpathia and allodynia, leading to the migraine headache phase. By inhibiting these inflammatory neuropeptides, acute interventions during a migraine attack can therapeutically modulate the symptoms. Preventive treatment measures aim to reduce sensitization in the trigeminocervical complex and to activate descending cortical pain control mechanisms.








It's wonderful to have family and friends who take these symptoms seriously. My whole life (I'm 58 now) I've had these symptoms and was never taken seriously; no one ever took me to the hospital in my condition. "You're not breathing properly, you're iron deficient, you're not resilient, don't act so silly, you're just faking it..." For me, these attacks were normal since childhood, and I thought it was somehow my own fault because the pediatrician couldn't find anything wrong. Later, it was endometriosis, iron deficiency, typical female hormones, etc. But I'm over all that now.
It wasn't until I was 56, after three car accidents, that the attacks became more frequent and without warning. I was finally taken seriously. Many tests followed. Now I'm seeing a neurologist, still trying to determine whether it's migraine with brainstem aura or some kind of epilepsy, since an anti-epileptic medication helps somewhat. In any case, the attacks are becoming less frequent, and I finally feel like I'm being taken seriously.
Now, at last, the people around me believe that I'm not imagining it or faking it, and they're suddenly concerned.
An impressive and very moving television report on NDR. Thank God the Kiel Pain Clinic exists.
Anyone who wants to can understand that, I can't.
beeper
I'm certain I don't have a brainstem aura, but I've often wondered if the pain in the back of my head—usually accompanied by dizziness and nausea—is also migraine. I've had migraine attacks of varying intensity and frequency since puberty, for almost 60 years now.
Now I'm almost certain that's the case, and that recently the brainstem nerves, and not just the trigeminal nerve, are affected.
For a while, I thought it might be due to spondylarthrosis in the last cervical vertebra.
My neurologist said that if triptans help, it's migraine. So I tried triptans, which do work.
Now I'm receiving Ajovy injections and hoping for a preventative effect (only for the last two months).
Best regards
Anna Schmitz