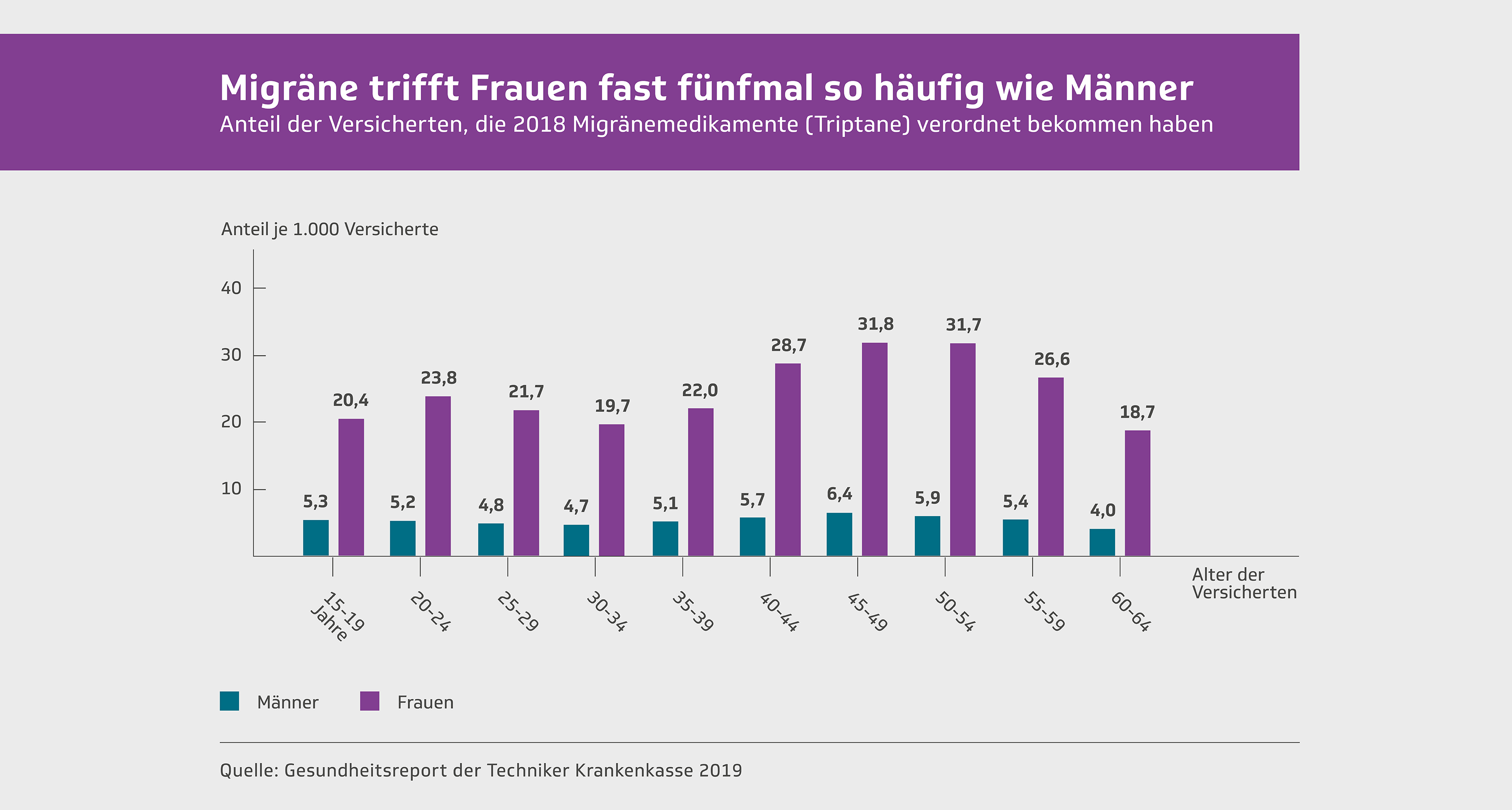
Migraines occur two to three times more often in women than in men. Migraines are the leading cause of disability in women aged 15 to 49. They have a significantly greater impact on women's careers than on men's. No other disease is responsible for more lost healthy years of life for women during their working years. Migraines are not only more common in women, but the attacks are also more severe. They last longer, the accompanying symptoms are more intense, and they respond less well to treatment. Many aspects of a woman's life must be considered when treating migraines.
The so-called menstrual migraine
The term "menstrual migraine" appears in many publications on the subject of headaches. It is used so routinely that for many years hardly anyone questioned it. In some cases, it was even believed that migraines were always somehow connected to menstruation. Migraines were perceived as a women's disease .
However, research has shown that the seemingly self-evident connection between female hormones, menstruation, pregnancy, menopause, birth control pills and migraines needs to be put into perspective.
Migraine attacks that occur exclusively during menstruation are extremely rare . After thorough questioning, those affected almost always recall that they suffer from migraine attacks not only during menstruation, but also at other times in their cycle.
The term "menstrual migraine" would only be meaningful if it referred to migraine attacks that occur exclusively in connection with menstruation. If one includes the three days before and after menstruation in the menstrual period, it becomes clear that at most one in 20 women who meet the criteria for migraine belong to this group. Therefore, the term "menstrual migraine" is only applicable to a small proportion of affected patients.
Likewise, a connection with the so-called premenstrual syndrome has not yet been scientifically proven. This syndrome, characterized by abdominal pain, weakness, and other psychovegetative symptoms, appears approximately two to three days before menstruation.
Migraine attacks occurring in temporal relation to menstruation are no different from other migraine attacks, even though menstrual migraine is often understood to be a particularly severe and prolonged attack accompanied by intense nausea and vomiting. However, any form of migraine, with or without aura, can occur during menstruation. If menstruation is indeed a trigger, the migraine attack is usually triggered two days before menstruation begins.
In patients who experience migraine attacks exclusively during menstruation, there is often a fixed temporal relationship between the attacks and menstruation. However, in other women, this temporal relationship can be loose, and the migraine attack can occur at varying intervals from menstruation.
Link between menstruation and migraines
Clinical and experimental studies have shown that migraines associated with menstruation are triggered by a drop in estrogen and progesterone levels . Accordingly, the decrease in plasma estradiol levels is likely responsible for triggering migraine attacks. Absolute hormone levels, on the other hand, do not appear to be significant. A possible cause of headaches during the estradiol drop is thought to be the hormone's effect on blood vessels, specifically vasodilation due to the lower hormone concentration. Further analyses of hormone concentrations have so far yielded no consensus on the significance of the various hormones in triggering migraine attacks. Neither follicle-stimulating hormone (FSH) nor luteinizing hormone (LH) levels differ between patients suffering from menstrual migraine and healthy controls.
Treatment of menstrual migraine
Due to the temporal correlation with menstruation, hormonal therapy seemed a logical approach. Previously, the administration of estrogen three to ten days before menstruation was recommended. However, it has been shown that this only delays the onset of the migraine attack until the natural drop in hormone levels occurs again.
The use of hormone patches that release estrogen through the skin has also proven ineffective in controlled studies. The same applies to the administration of estrogen in tablet form.
Pregnancy and migraine
Mutual influence
Migraines are of particular importance for a planned or existing pregnancy due to the following questions:
- How is migraine treated during pregnancy?
- Which medications are indicated or contraindicated?
- Is the pregnancy threatened by the migraine condition?
What effects can pregnancy have on the course of a migraine attack?
Fortunately, it has been observed that pregnancy has a very positive influence on the course of migraines. In fact, there is hardly a better preventative measure.
Epidemiological studies have shown that almost 70% of affected patients experience a significant improvement or even a complete cessation of migraine attacks during pregnancy. This effect on the course of migraines is particularly evident in the last two trimesters of pregnancy. Whether this positive effect on migraines gradually diminishes with subsequent pregnancies has not yet been clarified by studies.
Only a small percentage of patients experience a stable course or even a worsening of their migraine during pregnancy. This seems to be particularly true for patients suffering from migraine with aura. If migraine attacks occur for the first time during pregnancy, they are predominantly migraine with aura. However, this is only the case for a minority of those affected; according to a French study, it was 13% of the patients examined. After delivery, approximately half of the patients experience a recurrence of headaches in the first week, primarily tension headaches, but also migraine attacks.
Improvement in the course of migraines
The reason for the sometimes spectacular improvement during pregnancy is still completely unknown. However, various hypotheses are being discussed:
- On the one hand, it is assumed that the constantly elevated concentrations of estrogen and progesterone during pregnancy cause the improvement.
- Other explanations suggest that an altered serotonin metabolism during pregnancy and an increased concentration of endogenous opioids, i.e., opiate-like substances produced by the body itself, are responsible for the improvement.
- The altered lifestyle during pregnancy appears to play a crucial role. Pregnant women tend to eat more consciously, maintain a regular sleep-wake cycle, avoid alcohol and nicotine, try to live a less stressful life, and are less stressed at work. There is a pregnancy-related control of trigger factors, resulting in fewer migraine attacks. However, there are no empirical studies to confirm this hypothesis.
Migraine prophylaxis during pregnancy
Generally speaking, medication should be avoided during pregnancy whenever possible. This is especially true for prophylactic measures that require daily medication. Migraine prophylaxis medications that have proven particularly effective are contraindicated during pregnancy. This includes beta-blockers, flunarizine, serotonin antagonists, tricyclic antidepressants, and especially antiepileptics. This is particularly important if pregnancy is planned or even suspected. Since young women often use such medications for severe migraines, they must be advised of the necessity of adequate contraception.
To prevent migraine attacks during pregnancy, behavioral measures are recommended, as is generally the case, such as..
- Relaxation exercises and
- Identifying and avoiding trigger factors.
- In cases of severe migraine during pregnancy, especially migraine with aura, magnesium be considered for migraine prophylaxis. While clinical studies have generally shown that magnesium has a small effect on the course of migraines, a significant effect can be achieved in individual cases.
- Propranolol is used to treat arterial hypertension during pregnancy. There is no evidence of a risk of fetal abnormalities. Nevertheless, the use of propranolol for migraine prophylaxis during pregnancy should be approached with great caution and considered only as a last resort.
Treatment of migraine attacks during pregnancy
There is very little literature on the efficacy and tolerability of medications for treating migraine attacks during pregnancy. The same applies to the effects of medication-based migraine therapy on childbirth and breastfeeding.
Non-steroidal anti-inflammatory drugs such as ibuprofen or diclofenac should only be used in exceptional cases and exclusively in the second trimester of pregnancy.
Paracetamol was long considered the first-line analgesic during pregnancy, but it is increasingly being linked to later health problems in the child (increased risk of asthma, impaired psychomotor development, or cryptorchidism in boys). However, current data do not yet allow for a definitive assessment of the risks. Given the limited efficacy of paracetamol in treating migraines, its use during pregnancy is currently no longer recommended (see below).
not during pregnancy . Firstly, there is insufficient experience with their use, and secondly, it has not been proven that they are more effective at ending migraine attacks than the aforementioned substances that have been used for many decades. Particular care must be taken to ensure that NSAIDs are not used continuously. Especially during the last trimester, this can lead to a prolonged pregnancy, an increased risk of preeclampsia, an increased risk of bleeding for both mother and child, and an increased risk of persistent pulmonary hypertension in the child.
Warning about paracetamol during pregnancy
New studies describe a possible link between exposure to paracetamol before birth and an increased risk of asthma, other respiratory diseases, and impaired testicular development.
Paracetamol was previously considered the safest pain reliever during pregnancy. Based on earlier data, its safety seemed beyond doubt. Pregnant women were advised to take this pain reliever for pain during pregnancy with virtually no concerns. However, current studies necessitate a careful reassessment of this recommendation. New studies describe a possible link between exposure to paracetamol before birth and an increased risk of asthma, other respiratory illnesses, and impaired testicular development. Psychomotor developmental disorders in the child are also being discussed. Contrary to previous recommendations, the use of paracetamol, both as a single-ingredient product and especially in combination preparations, is therefore discouraged in cases of suspected or confirmed pregnancy.
Until the exact connection is clarified, the principle must apply: when in doubt, choose the unborn life and advise against taking paracetamol, especially in combination with other painkillers.
Based on the new data, the short-term benefits and long-term lifelong risks are no longer in balance with each other in the case of a possible or existing pregnancy.
The use of paracetamol by pregnant women and the unborn child's exposure to the drug appears to significantly increase the risk of developing asthma and respiratory diseases in their children, as well as potential infertility in boys. In recent years, there has been a marked global increase in the prevalence of asthma. Paracetamol is one of the most frequently used medications in Germany. Paracetamol can lead to a reduction in glutathione levels in the lungs. Glutathione is believed to play a significant role in the development of asthma.
Particularly concerning, according to new study results, is the well-founded suspicion of a significantly increased risk of developing cryptorchidism (undescended testicles) in boys. This can later lead to reduced fertility and an increased risk of developing testicular cancer. Sperm count and viability may also be reduced later in life. The combined use of two painkillers in pregnant women was associated with a sevenfold increased rate of cryptorchidism in newborn boys. It is suspected that the effects of a single 500 mg paracetamol tablet on the unborn child could be more harmful than the ten most common environmental pollutants. These studies have been criticized for not definitively proving a causal relationship.
Paracetamol, in therapeutic doses, has long been considered a safe, harmless, well-tolerated, and inexpensive pain reliever. However, the risk of irreversible liver cell damage leading to liver failure in overdoses exceeding 150 mg per kg of body weight has already led to limitations on package sizes for self-medication. New studies have prompted a significant reassessment of its use in cases of possible, planned, or existing pregnancy.
Generally, painkillers should be avoided during pregnancy and breastfeeding. In individual cases of particularly severe pain, acute medication may be considered after consulting a doctor. However, it should be noted that so-called simple painkillers such as paracetamol have only a weak and short-term effect on severe pain attacks, while simultaneously posing lasting lifelong risks to the unborn child.
Contrary to previous recommendations, the use of paracetamol in mono- and especially combination preparations is therefore discouraged in the case of possible or existing pregnancy.
Triptans
The company pregnancy registry has so far not shown a significantly increased risk of birth defects when sumatriptan is used in the first trimester of over 1000 pregnancies.
For the remaining triptans, there is insufficient data to assess their safety during pregnancy. Until sufficient experience is available, triptans should not be used during pregnancy.
Ergot alkaloids, such as ergotamine tartrate and dihydroergotamine, are strictly contraindicated. These substances have a uterotonic effect during pregnancy. Furthermore, ergotamine is toxic to the embryo.
Treatment of migraine attacks during breastfeeding
Painkillers
Ibuprofen is the analgesic of choice during breastfeeding. With occasional use, only very small amounts pass into breast milk and it is even approved for the treatment of newborns.
Triptans
Triptans pass into breast milk. The product information recommends a 12-hour waiting period after taking sumatriptan and a 24-hour waiting period for all other triptans.
Behavior when trying to conceive
- In the first 14 days after the first day of the last menstruation (assuming a regular 28-day cycle!), it can be assumed that there is no pregnancy.
- In a regular cycle, ovulation occurs approximately 14 days before menstruation.
- Six days after ovulation, the fertilized egg implants in the uterus, thus marking the first contact between "mother and child".
- Medication to treat migraine attacks is possible for approximately the first three weeks after the first day of the last menstruation without endangering the fetus.
- An existing pregnancy can be detected with newer pregnancy tests from the 6th to 10th day after ovulation; this means that there are some "uncertain" days about three weeks after menstruation, during which it is recommended to take a pregnancy test before taking any acute medication.
Birth control pill and migraine
In cases of persistent migraine attacks that are difficult to treat, the birth control pill is often blamed as a trigger. However, empirical investigations into a link between the birth control pill and migraines show no clear connection: some studies report an increased incidence of migraine attacks, with this occurring in 18–50% of affected patients, depending on the study. In contrast, other studies show an improvement in migraines in up to 35% of patients treated with the birth control pill. However, so-called double-blind studies have found no significant difference between groups of patients treated with the birth control pill and those treated with a placebo.
All in all, it appears that there is no definitive link between the birth control pill and migraines.
Migraine treatment is the same whether or not a woman is taking birth control pills. There is also no known interaction between birth control pills and migraine medications. The same guidelines apply to migraine therapy as for other conditions.
Only in rare cases of migraine that do not respond to medication is a trial discontinuation of the birth control pill advisable. Patients should then be advised to use an alternative method of contraception.
Due to the increased risk of arterial or venous cerebral thrombosis and cerebral hemorrhage, a neurological examination should be arranged as soon as possible in the event of the sudden onset of neurological disorders. This also applies to unexplained headache attacks. For this reason, patients taking birth control pills should be monitored more frequently to assess the course of the disease. Smoking should be strictly avoided. This is especially important due to the potentially increased risk of stroke associated with migraine. However, the overall risk of stroke in migraine is extremely low. Therefore, migraine is by no means a contraindication for the use of oral contraceptives.
Menopause and advanced age
It is often believed that migraines gradually "burn out" in old age, meaning they decrease in frequency and intensity. However, studies addressing this issue show that more than 50% of those affected no change in their migraine pattern . In fact, about 47% of female patients even experience a worsening of their condition.
The higher frequency of migraines in women compared to men persists into old age. Hormone therapies in old age cannot influence migraines. Therefore, in this age group, migraine therapy should be carried out as usual.
Beyond the age of 75 or 80, however, a change seems to occur. In fact, there are hardly any patients older than 80 who complain of migraine attacks in specialized migraine clinics.










Leave a comment