How do corticosteroids used for migraine, cluster headaches, and other headaches affect the SARS-CoV-2 vaccination?
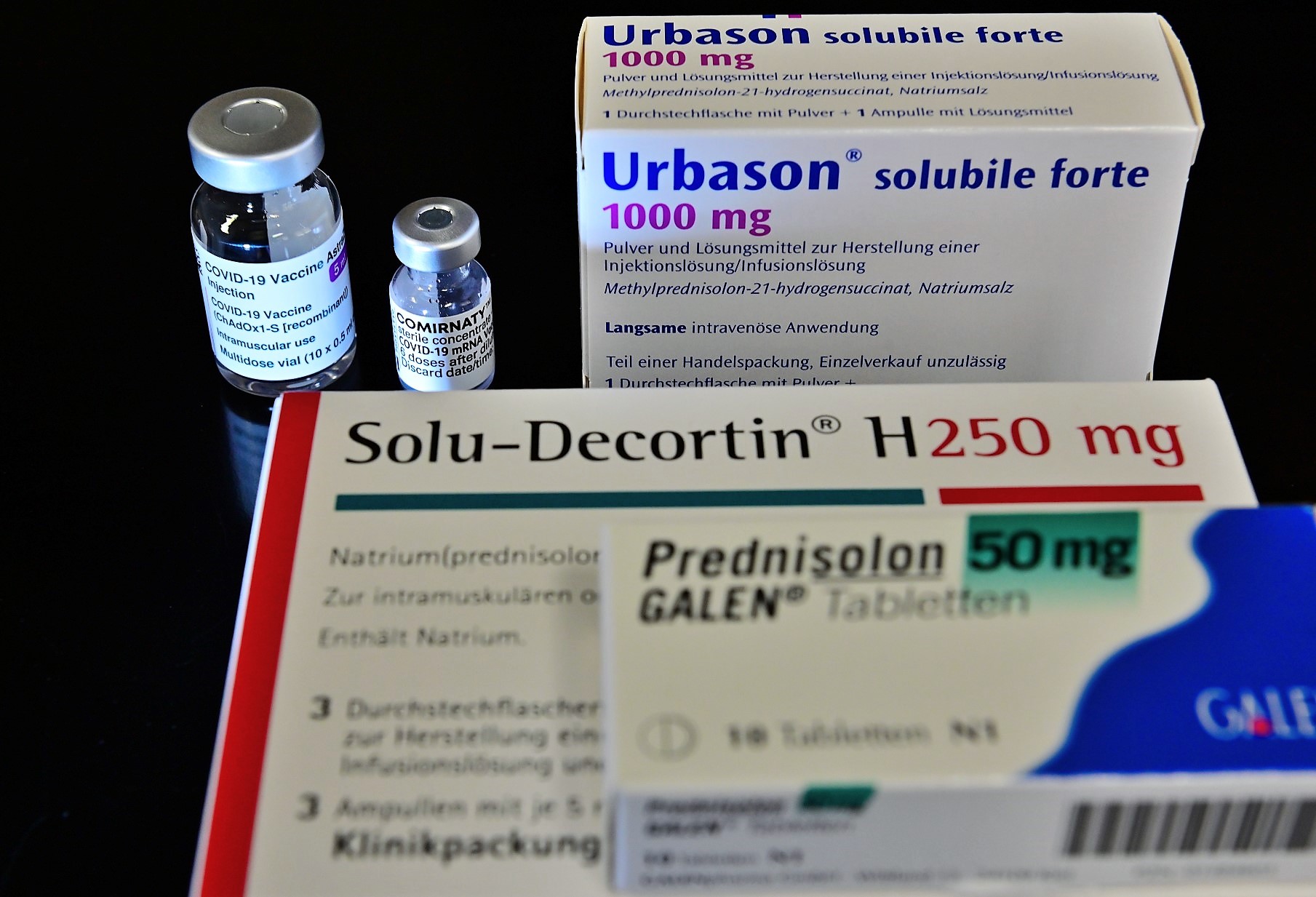
- Therapy with prednisolone and other corticosteroids (“cortisone”), e.g., for the treatment of status migrainosus, cluster headaches, or for the treatment of rebound headaches during a medication break for medication overuse headache (MOH), should not be carried out for approximately 8 weeks before to 2 weeks after vaccinations with live vaccines.
- However, the vaccines currently approved against SARS-CoV-2 are not live vaccines . Such non-live vaccines can be used without restriction in patients with migraines and other headaches.
- Classical non-live vaccines (inactivated vaccines) that are under development for vaccination against SARS-CoV-2 are vaccines based on adjuvanted proteins.
- Vaccines based on non-replicating vectors (AstraZeneca) and mRNA vaccines (e.g., BioNTech/Pfizer and Moderna) are distinguished from live vaccines. Their use is the same as that of inactivated vaccines.
- Vaccinations with such inactivated vaccines are generally possible for migraines, cluster headaches and other headaches.
- However, it should be noted that the immune response, and therefore the success of the vaccination, can be impaired at higher doses of corticosteroids. For fundamental reasons related to the effectiveness of a vaccination, the dosage of corticosteroids at the time of vaccination should therefore be as low as possible.
- The approval studies do not provide any findings for treatments with immunomodulating/immunosuppressive therapies such as corticosteroids.
- Treatment with corticosteroids can fundamentally affect the immune response to vaccinations. Therefore, vaccinations against Covid-19 should be administered no sooner than two weeks, and preferably four weeks, after treatment with corticosteroids.
- Corticosteroids should only be used after 14 days following vaccination in order to avoid reducing the vaccine response.








Leave a comment