On November 29, 2017, the results of two studies on the effectiveness of antibodies against CGRP in preventing chronic and episodic migraines were published in the New England Journal of Medicine 1,2 . The antibody therapy targets a molecule that plays a key role specifically in inflammation, sensitization and pain during migraine attacks. The current facts are summarized below.
Current facts about migraines
- Migraine is the third most common disorder in the world (behind dental caries and tension headaches) with an estimated global one-year prevalence of 14.7%. This means that around one in seven people suffers migraine attacks within a year. Almost every third woman between the ages of 30 and 40 is affected.
- Migraines are more common than diabetes, epilepsy and asthma combined.
- Chronic migraine affects approximately 2% of the world's population. The World Health Organization (WHO) estimates that between 127 and 300 million people worldwide suffer from chronic migraine.
- Migraines affect three times as many women as men.
- 900,000 people in Germany are affected every day. 100,000 people are unable to work and bedridden every day because of migraines.
- On average, 8.3 million Germans take a headache tablet every day through self-medication.
- On average, 58,853 individual doses of triptan, which are special migraine medications for treating migraines, are taken every day in Germany
- More than half of those affected experience severe impairment as a result of the attacks.
- Migraines often begin during puberty. It is most disabling between the ages of 35 and 45. But many young children are also affected. In recent years there has been a strong increase, particularly among children.
- Migraine is the seventh most debilitating disease worldwide and the leading cause of disability among all neurological diseases.
- It is estimated that the German population loses 32 million working days due to migraines.
- Severe migraine attacks are classified by the World Health Organization as one of the most disabling diseases, comparable to dementia, paraplegia, which affects all four limbs, including both legs and arms, and active psychosis.
- Migraines and chronic headaches are the second most common reason for short-term incapacity to work.
- Incapacity to work due to migraines alone costs 3.1 billion euros per year in Germany, calculated based on 32 million days lost.
- The risk of depression, anxiety disorders and suicide is 3 to 7 times higher in those affected than in healthy people.
- The risk of circulatory diseases, heart attack and stroke is 1.5 to 2 times higher than in healthy individuals. This is particularly true for young women under 45 years of age.
- It is scientifically proven that migraines have a genetic basis. 44 gene variants in 38 risk genes for migraine are now known.
- One of the most common health problems treated with scientifically unsupported unconventional therapies is headache.
- Worldwide, on average only about two to four hours of information about headache diagnosis and treatment are offered during the six-year medical course.
- Despite the proven effectiveness of using specialist nurses for headache treatment, there is no specialized training in Germany.
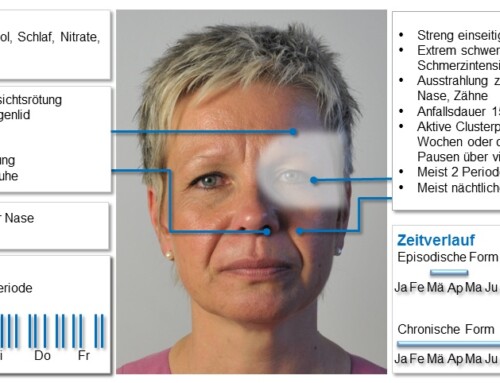
- Migraine and other headaches were first classified internationally in 1988 by the International Headache Society (IHS) and operationalized diagnostic criteria were described. The International Classification of Headache Disorders, 3rd Edition (ICHD-3) beta was published in 2013. It is recognized by the World Health Organization. Researchers and clinicians worldwide refer to these internationally valid diagnostic criteria. Today there are 367 main diagnoses of headaches. No other neurological disease has a comparable, differentiated diagnosis and classification system.
The facts about migraine development
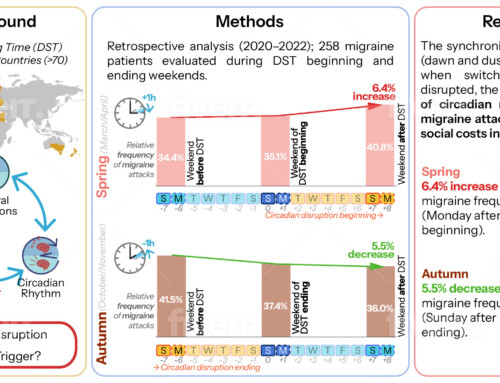
Today it is known that migraine patients have numerous special genetic characteristics. There are now 38 gene loci with 44 gene variants known that increase the risk of migraines. On the one hand, these gene variants control stimulus transmission, stimulus sensitivity and stimulus processing. On the other hand, these gene variants also control the regulation of the energy supply to nerve cells and the regulation of the artery walls. Arterial walls should not be thought of as a kind of lifeless tube. Rather, the coverings of the blood vessels are the largest endocrine organ in our body. Numerous messenger substances are produced here that regulate blood circulation and inflammatory reactions. Many substances are also activated there that are relevant for important control processes in our body. A disruption in the energy supply, for example due to oxidative stress, can bring this regulation into imbalance and cause malfunctions. Hereditary factors as well as environmental, behavioral and social factors play a significant role in the development of migraine attacks.
The peculiarities of migraine systems mean that those affected can perceive stimuli very intensely. They are also able to differentiate between stimuli in a very active and differentiated manner. If stimuli occur repeatedly, migraine patients do not get used to them, but can absorb them in a very differentiated manner; so-called stimulus adaptation and distraction from stimuli hardly takes place. The result is that migraine sufferers can, metaphorically speaking, hear the faucet dripping three rooms away. You already have answers to questions that no one has asked yet. They color thoughts and perceptions much more intensely with emotions. They notice changes in the environment very quickly. For example, if a picture is hanging crooked on the wall, they notice this immediately and feel the impulse to straighten it. This quick and active communication of stimuli can also lead to very significant achievements. Many famous people who have achieved great things also suffered from migraines. Examples include Marie Curie, who suffered from severe migraine attacks almost daily as a student and later became the only person to receive a Nobel Prize in two scientific fields. Richard Wagner set his own migraine to music in the first bar of his opera “Siegfried” and translated the pulsating and pounding headache into sounds and even created a musical monument to his visual migraine aura. Vincent van Gogh also brought to the screen how seeing during the visual aura changes perception. Other examples include Charles Darwin, Alfred Nobel, Salvador Dali, Claude Debussy, Frederic Chopin and many others. It is important that you deal with this special “operating system” in such a way that your own behavior and lifestyle enable you to work as smoothly as possible. The most important rule is regularity and synchronicity, so that anything too fast, anything too many, anything too sudden and anything too impulsive can be avoided in everyday life, thereby preventing over-stimulation and exhaustion of nervous energy.
Facts about CGRP
For the first time, it has been possible to develop specific antibodies against messenger substances that cause inflammation in the arteries of the meninges. If you give so-called monoclonal antibodies, the effects of these inflammatory substances can be stopped for a few weeks and the likelihood of migraine attacks can be significantly reduced. The so-called CGRP, an inflammatory protein, plays a central role. Four antibodies are currently being developed and tested in numerous studies.
The antibodies now available have all proven their effectiveness in very large international studies. There are antibodies that work directly against CGRP or block the receptor for CGRP. They must be administered approximately 4 weeks apart.

The antibody (blue) against the CGRP receptor (orange) blocks and protects it from CGRP. CGRP can no longer reach it, activate it and trigger inflammation and pain.
In contrast to all other preventative medications available to date, the new immunotherapy has been developed specifically for migraine prevention for the first time. A slow dosage increase due to intolerances and side effects is not necessary. The onset of effect can be expected quickly within a few days; with conventional preventive medications, this is often only achieved after weeks or even months. Side effects of previous migraine preventatives such as weight gain, mood changes, fatigue, reduced drive or drowsiness do not occur. In contrast to previous medications, which are often discontinued after a short period of time due to such side effects, the treated patients stick with this therapy principle for the long term due to its tolerability and effectiveness.
Fremanezumab reduces migraine frequency in phase 3 study in chronic migraine
Prophylactic administration of fremanezumab significantly reduces the number of headache days per month in patients suffering from chronic migraine. The substance can be given one month apart or three months apart. in a phase 3 study published 1
The study included 1,130 patients suffering from chronic migraines. In chronic migraine, headaches occur on more than 15 days per month, with at least 8 days corresponding to the typical picture of migraine attacks. The patients were randomly divided into three equal groups. The first group received 675 mg of fremanezumab as a single dose at the start of treatment, and a drug-free substance (placebo) was injected at intervals of 4 and 8 weeks. The second group received 675 mg of fremanezumab at the beginning, followed by 225 mg of fremanezumab every 4 and 8 weeks. The third group was treated with a drug-free placebo at the respective time points.
After 12 weeks, the reduction in headache days per month by at least 50% was examined. The percentage of patients who achieved this reduction of at least 50% in their attack frequency was:
- 38% in the group that received fremanezumab quarterly
- 41% in the group that received fremanezumab with monthly treatment and
- 18% in the placebo group.
Placebo was significantly inferior in efficacy in both groups (P < 0.001).
Adverse events were reported in 64% of patients receiving placebo, 70% of patients receiving quarterly fremanezumab, and 71% of patients receiving fremanezumab monthly. Adverse events were of mild to moderate intensity in 95-96% of patients in the 3 groups. The most common side effects were pain at the injection site. These occurred in 30% of patients receiving fremanezumab every three months, 26% receiving fremanezumab monthly, and 28% of patients receiving placebo. Adverse events led to discontinuation of the study in 1% of the quarterly group, 2% in the monthly group and 2% in the placebo group.
Patients may continue treatment with the antibody after completion of the double-blind study to analyze efficacy and safety over long-term use. The study results are consistent with previous dose-finding studies in chronic migraine. The authors express that further studies are needed in patients with migraine and its common comorbidities.
Erenumab shows attack reduction in phase 3 study in episodic migraine.
In the same issue of the New England Journal of Medicine on November 29, 2017, new data on erenumab in the prevention of episodic migraines are also published. Erenumab was administered subcutaneously at 4-week intervals at a dosage of 70 mg or 41 mg. The analysis showed that the antibody significantly reduced the frequency of migraines, the effect of migraines on daily activities and the need for the use of acute migraine medications over a 6-month period.
955 patients were treated in the study. 317 received erenumab 70 mg, 319 erenumab 140 mg and another 319 patients received drug-free placebo treatment. At the start of the study, the mean frequency was 8.3 migraine days per month.

Rate of at least 50% reduction in migraine days per month compared before treatment with the frequency during the double-blind treatment phase (2)
The efficacy parameters were analyzed after 4-6 months of treatment. The following results were shown:
The number of migraine days was reduced by
- 3.2 days in the 70 mg erenumab group
- 3.7 days in the 140 mg erenumab group
- 1.8 days in the placebo group (P < 0.001 for any dose versus placebo)
A greater than 50% reduction in the mean number of migraine days per month was achieved for
- 43.3% of patients in the 70 mg erenumab group
- 50% of patients in the 140 mg erenumab group
- 26.6% in the placebo group (P < 0.001 for any dose versus placebo)
The number of days with the need to take migraine acute medication was reduced to
- 1.1 days in the 70 mg erenumab group
- 1.6 days in the 140 mg erenumab group
- 0.2 days in the placebo group (P < 0.001 for any dose versus placebo)
Physical disability improved by the following scores:
- 4.2 points in the 70 mg erenumab group
- 4.8 points in the 140 mg erenumab group
- 2.4 points in the placebo group (P < 0.001 for each dose versus placebo)
Daily activities improved in terms of the analyzed scores by:
- 5.5 points in the 70 mg erenumab group
- 5.9 points in the 140 mg erenumab group
- 3.3 points in the placebo group (P < 0.001 for each dose versus placebo)
The frequency and severity of adverse events were approximately equal between the erenumab and placebo groups.
The authors conclude from these data that erenumab may be an effective substance in the prevention of episodic migraine. Further studies are needed to analyze long-term safety and tolerability. The long-term effectiveness and sustainability of the clinical effects also need to be broken down in more detail in further studies.
And what do the results mean for care?
The extensive analyzes show that the new substances only have a clinical effect for some patients. If you look at the mean values regarding the reduction in headache days per month, the changes compared to the placebo effect are significant but clinically in similar areas as the preventative medications already available. Migraine attacks may continue to occur.
On average, their frequency can be reduced by around 25% compared to placebo. However, there are also patients who respond very well to the treatment and whose headaches almost completely stop. This effect can be explained by the fact that CGRP is only one of several transmitters that are important in the development of migraines.
This is also to be expected. If at least 38 risk genes and 44 gene variants are responsible for the different mechanisms in migraine, there is a complex basis with various pathways in the nervous system to generate migraine attacks. Patients for whom CGRP is a primary concern can hope for significant relief with appropriate treatment.
Other affected people, for whom other mechanisms are in the foreground, will have to wait for future therapy developments.
However, for the first time in human history, the new substances enable specific prevention of migraines by directly intervening in the mechanisms that cause them. While previous migraine medications only accidentally demonstrated their effectiveness when used in other diseases, the new antibodies were developed specifically to prevent migraines. They open up new hope for patients who have not yet been able to receive sufficient help. The advantage is that the new antibodies work outside the blood-brain barrier and therefore central nervous side effects such as fatigue, dizziness, changes in emotions and weight gain are not to be expected.
Although some patients experienced a 100% reduction in attack frequency, other patients did not respond to treatment. The degree of effect varies greatly between treated study participants.
The new findings show that a new door has historically been opened to the treatment of migraines. If the previous data is confirmed, more patients will be able to reduce their migraine burden and return to a normal life in the future.
The desire to eliminate the attacks without adapting your life to your migraine predisposition can also be dangerous. The dream of not having to observe the most important preventative rule, namely paying attention to regularity and synchronicity in order to be able to live as one wants without restrictions, can become a problem. Anything too fast, anything too many, anything too sudden and anything too impulsive then causes over-stimulation and exhaustion of the nervous energy. Over time, this can cause psychological and physical complications. Complex development mechanisms therefore continue to require comprehensive treatment.
It's like a flat bicycle tube that has five holes. If you just patch one thing, the air will be out the next morning. You have to find all five leaks and patch them at the same time so you can get going.
literature
1 Silberstein SD, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med 2017;377:2112-22. http://www.nejm.org/doi/full/10.1056/NEJMoa1709038
2 Goadsby PJ, et al. A controlled trial of erenumab for episodic migraine. N Eng J Med 2017;377:2123-32. http://www.nejm.org/doi/full/10.1056/NEJMoa1705848






Thank you for these very informative posts. I can understand everyone who suffers from migraines very well, as I have suffered from it myself for 53 years. I've tried everything possible now, but with little success. I really hope that this new drug will be officially approved in Germany as soon as possible and will therefore be available to everyone. It would also be desirable for the health insurance companies to cover the resulting costs financially!
Marlene Kempel:
My biggest concern is that I can no longer take the triptans because I suffer from coronary heart disease. At the moment I'm just going to keep taking them because regular painkillers, even in high doses, don't help. I'm constantly looking for alternatives, but so far I haven't found anything that can permanently and effectively curb the pain. In the meantime I could write a book about the many experiments. Apart from the immense costs that I have often borne myself up to now, I am very disappointed when there is no improvement at all.
I have been suffering from migraines for 30 years and am very happy about the progress in medicine. Hopefully the drug will be used soon. I've been retired for 4 years because of my migraines.
A glimmer of hope in the complex migraine chaos, one can only thank the people who are researching the migraine scourge so intensively.
But how do you get a study participation or treatment?
In any case, I am very happy about the very good contribution.
Olaf Biewald
I, Monika Kornberger, was in inpatient treatment at the Kiel Pain Clinic in Kiel in 2014.
I've been suffering from migraines since I was 27. I am now 65 years old and still have severe migraines.
I'm not pain-free for a day anymore. Trigeminal neuralgia has now been diagnosed, predominantly on the right and starting on the left. I have n't given up hope for an improvement yet. I have a very bad headache, along with tinnitus.
I have balance problems. Because of the pain, I don't socialize as much anymore. I would be very grateful if this new medication would help.
Thank you for the detailed and, above all, understandable presentation of the CGRP development in this newsletter from December 2017. Perfect for Christmas: the big door is about to open.
Although anticipation is not the greatest, there is hope for a positive effect and that is something. Merry Christmas and a hopeful 2018.
Thank you for clearly explaining the effects of migraines. So far I have never read or heard such a description anywhere. I feel really understood and taken seriously. It would be nice if the above description “Severe migraine attacks are classified by the World Health Organization among the most disabling diseases, comparable to dementia, paraplegia, in which all four limbs, i.e. both legs and arms, are affected, and active psychosis.” would have a corresponding impact in assessing disability, pension applications, etc. And it would be even better if one of the new remedies could help me. Thank you very much for your effort.
That gives hope. I hope that the antibody treatment can be used based on my medical history. Relief after 39 years of migraines!?
Very hopeful. It would be very desirable to have such a drug available. A new life for me after 43 years of migraines.