Die Schmerzklinik Kiel erreichen täglich hunderte Anfragen zu einem möglichen Zusammenhang zwischen einer Impfung gegen Covid-19 und dem Vorgehen bei einer parallel bestehenden Migränebehandlung. Hier die wichtigsten Antworten:
Was weiß man zu Wechselwirkungen zwischen Impfungen gegen Covid-19 und gleichzeitiger Migränetherapie?
Aktuell sind keine Ergebnisse aus Studien bekannt, dass es Wechselwirkungen oder Komplikationen zwischen Impfung gegen COVID-19 und einer zusätzlich bestehenden vorbeugenden Migränebehandlung oder einer Akutbehandlung der Migräneattacke gibt.
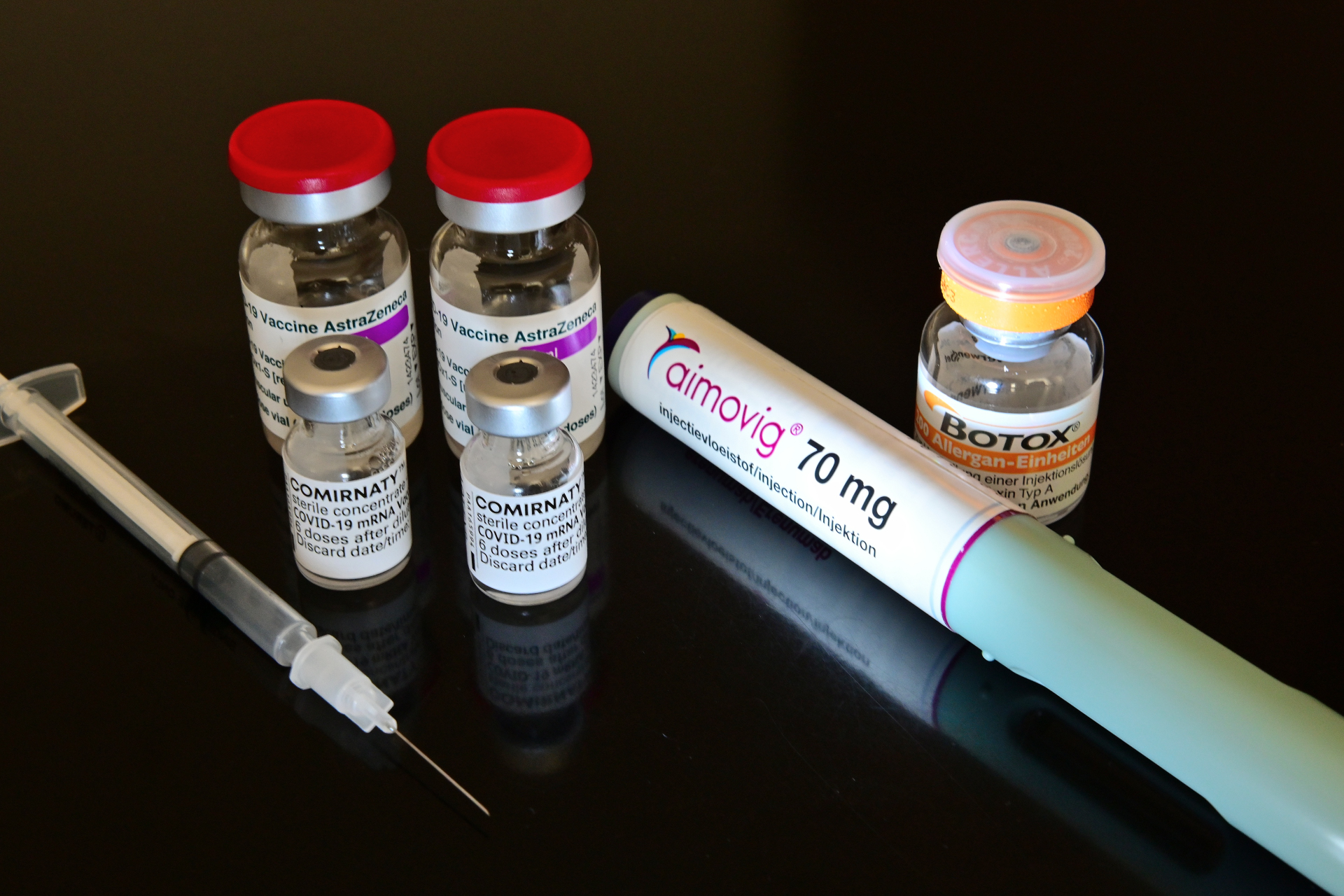
Gilt dies auch für Onabotulinumtoxin A (Botox) -Injektionen und CGRP-monoklonale Antikörper?
Dies gilt sowohl für Onabotulinumtoxin A (Botox) -Injektionen als auch für die Anwendung von CGRP-monoklonale Antikörper.
Kann die Migränebehandlung die Impfwirkung abschwächen?
Es gibt aktuell keine Datengrundlage, dass die Migränebehandlung die Wirksamkeit oder Sicherheit der COVID-19-Impfstoffe beeinträchtigt. Ebenfalls gibt es keine Hinweise darauf, dass die Impfung gegen Covid-19 die Wirksamkeit der Migränebehandlung reduziert.
Es gibt bisher keine Daten, die zeigen, dass die durch den Impfstoff gebildeten Antikörper gegen das SARS-CoV-2-Spike-Protein das Medikament Onabotulinumtoxin A unwirksam machen würden. Dies gilt auch für die Medikamente Erenumab (Aimovig), Fremanezumab (Ajovy) oder Galcanezumab (Emgality).
Kann man Impfung und Migränebehandlung bedenkenlos gleichzeitig durchführen?
Dass etwas nicht bekannt ist oder noch nicht untersucht ist, bedeutet nicht, dass Risiken nicht bestehen und man bedenkenlos vorgehen kann. Dies gilt insbesondere für die Überlagerung von Nebenwirkungen bei gleichzeitiger Anwendung. Bedenken bestehen weniger wegen der Wirksamkeit als wegen möglicher Überlagerung von Nebenwirkungen.
Welche Nebenwirkungen können Covid-19-Impfstoffe haben?
Am Beispiel des BNT162b2-mRNA-Covid-19-Impfstoffs (BioNTech/Pfizer) sind die häufigsten Nebenwirkungen Reaktionen an der Injektionsstelle (84,1%), Müdigkeit (62,9%), Kopfschmerzen (55,1%), Muskelschmerzen (38,3%), Schüttelfrost ( 31,9%), Gelenkschmerzen (23,6%) und Fieber (14,2%).
Am Beispiel des ChAdOx1 nCoV-19 (AZD1222) AstraZeneca Impfstoffes sind die häufigsten Nebenwirkungen Schmerzen an der Injektionsstelle (54.2%), Kopfschmerzen (52.6%), Müdigkeit (53.1%), Muskelschmerzen (44.0%), Gelenkschmerzen (26.4%), Unwohlsein (44.2%), Übelkeit (21.9%), Schüttelfrost (31.9%) oder Fieber> 38 °C (7.9%). In den klinischen Zulassungsstudien zum AstraZeneca-Impfstoff wurde die Verwendung von Paracetamol vor der Impfung in allen Studien vorbeugend empfohlen (außer in der Studie COV005; sie wurde als Änderung während der Studie COV001 eingeführt). Den Geimpften wurde empfohlen, nach der Impfung 1000 mg Paracetamol einzunehmen und über 24-Stunden im Intervall von sechs Stunden vorbeugend fortzufahren, um durch den Impfstoff verursachte Nebenwirkungen zu verringern. Es ist daher anzunehmen, dass durch die prophylaktische Verabreichung von Paracetamol Nebenwirkungen wie Fieber und Kopfschmerzen gemildert wurden. Eine vorbeugende Behandlung von Kopfschmerzen nach der Impfung ohne Symptome ist nicht empfehlenswert.
Welche Nebenwirkungen können monoklonale Antikörper zur Migränevorbeugung haben?
Bei der Anwendung von monoklonalen Antikörpern zur Migränevorbeugung können am Beispiel von Erenumab (Aimovig) folgende Nebenwirkungen auftreten: Überempfindlichkeitsreaktionen, wie akute starke allergische Reaktion, die mehrere oder alle Körpergebiete betrifft (Anaphylaxie), spontan auftretende (Schleim-) Haut-Schwellung (Angioödem), Hautausschlag, Schwellung, Wassereinlagerung (Ödem), Nesselausschlag (Urtikaria), Verstopfung, Juckreiz (Pruritus), immunbedingter Hautausschlag mit Juckreiz, Muskelkrampf und Reaktionen an der Einstichstelle.
Kann man die Überlagerung von Nebenwirkungen reduzieren?
Da im Einzelfall auch ausgeprägte Nebenwirkungen auftreten können, empfehlen wir zur Vermeidung additiver Effekte bzgl. der Nebenwirkungen (Summation von Nebenwirkungen beider Arzneimittel) einen möglichst großen Abstand zwischen der Impfung gegen Covid-19 und der Gabe von monoklonalen Antikörpern zur Migränevorbeugung einzuhalten. Da die Gabe der monoklonalen Antikörper zur Migränevorbeugung in der Regel im Abstand von vier Wochen erfolgt, entspricht dies einem möglichen Abstand von 14 Tagen. Diese Empfehlung begründet sich auf die Vermeidung von überlagerten Nebenwirkungen aus beiden Anwendungsbereichen.
Was kann man gegen Kopfschmerzen nach der Impfung machen?
Treten Kopfschmerzen nach der Impfung auf, können diese mit Aspirin, Ibuprofen oder Paracetamol behandelt werden. Eine vorbeugende Behandlung von Kopfschmerzen nach der Impfung ohne Symptome ist nicht empfehlenswert.
Wie kann man Migräneattacken nach der Impfung behandeln?
Treten Migräneattacken nach der Impfung auf, können diese wie sonst auch mit der empfohlenen Akutmedikation (z.B. Triptane, Schmerzmittel) behandelt werden.






Ein sehr hilfreicher Kommentar, nicht nur für Migränepatienten. Danke dafür. Werde auch meinen Freundeskreis darüber informiren.
Danke für den Hinweis. Ich werde die Empfehlung bei der zweiten Impfung beherzigen. Ich hatte bereits die erste Impfung mit Astra und habe rein zufällig einen 12 tägigen Abstand zur CGRP-Spritze eingehalten. Bei Aimovig wie üblich fast keine Nebenwirkungen, bei Astra – Impfung ausgeprägte Abgeschlagenheit, Schwächegefühl, das sehr lange angehalten hat , sonst nichts, nicht mal Kopfschmerzen.