Generations of students have struggled with the problem that a word can have a different gender in different languages. The assignment to female, male or objective gender often seems rather arbitrary. A typical example is pain. dolore is derived from the Latin dolor in the same way as the French douleur - only the former is masculine and the latter feminine! Even with geographically neighboring languages such as Spanish and Portuguese, there is no agreement: the Spanish dolor is masculine, the Portuguese dor feminine. People were already at odds in ancient times. Unlike dolor in Latin, ἄλγος (algos) was neutral in ancient Greek! If pain is sometimes assigned to the female gender, sometimes to the male gender, and sometimes to no gender in different languages, this may simply reflect the experience that both genders can feel pain equally. It is all the more astonishing how uniform migraine, hemicrania, emicrania, migraine, migraña, enxaqueca or jaqueca is in the different languages of the female gender. In the opinion of the people, migraines are apparently predominantly a disease of women.
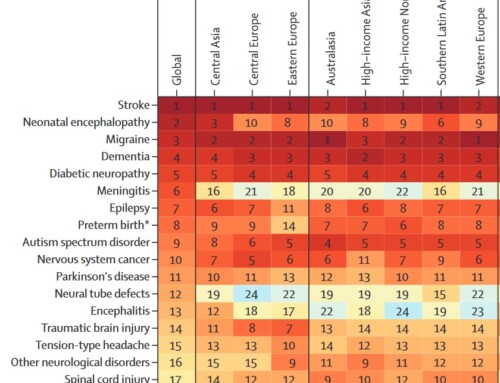
The question of whether this is actually the case can be approached epidemiologically. Representatively selected population samples actually show a female predominance by a factor of 2-3 over the entire lifespan (1). Before the age of 12, there is little difference between the two sexes. Among younger children, boys tend to be affected somewhat more often. This changes when you enter puberty. The abrupt drop in estrogen levels before menstruation is a potent trigger for migraine attacks in many women (2). It does not play a significant role whether it is the natural hormonal fluctuations or the estrogen withdrawal during the “pill break” when taking estrogen-containing contraceptives (3). It is not uncommon for a drop in hormones to be the only trigger in women. This female-specific menstrual migraine is probably the main reason why migraines occur more often in women than in men, but also why migraines are perceived as a female disease.
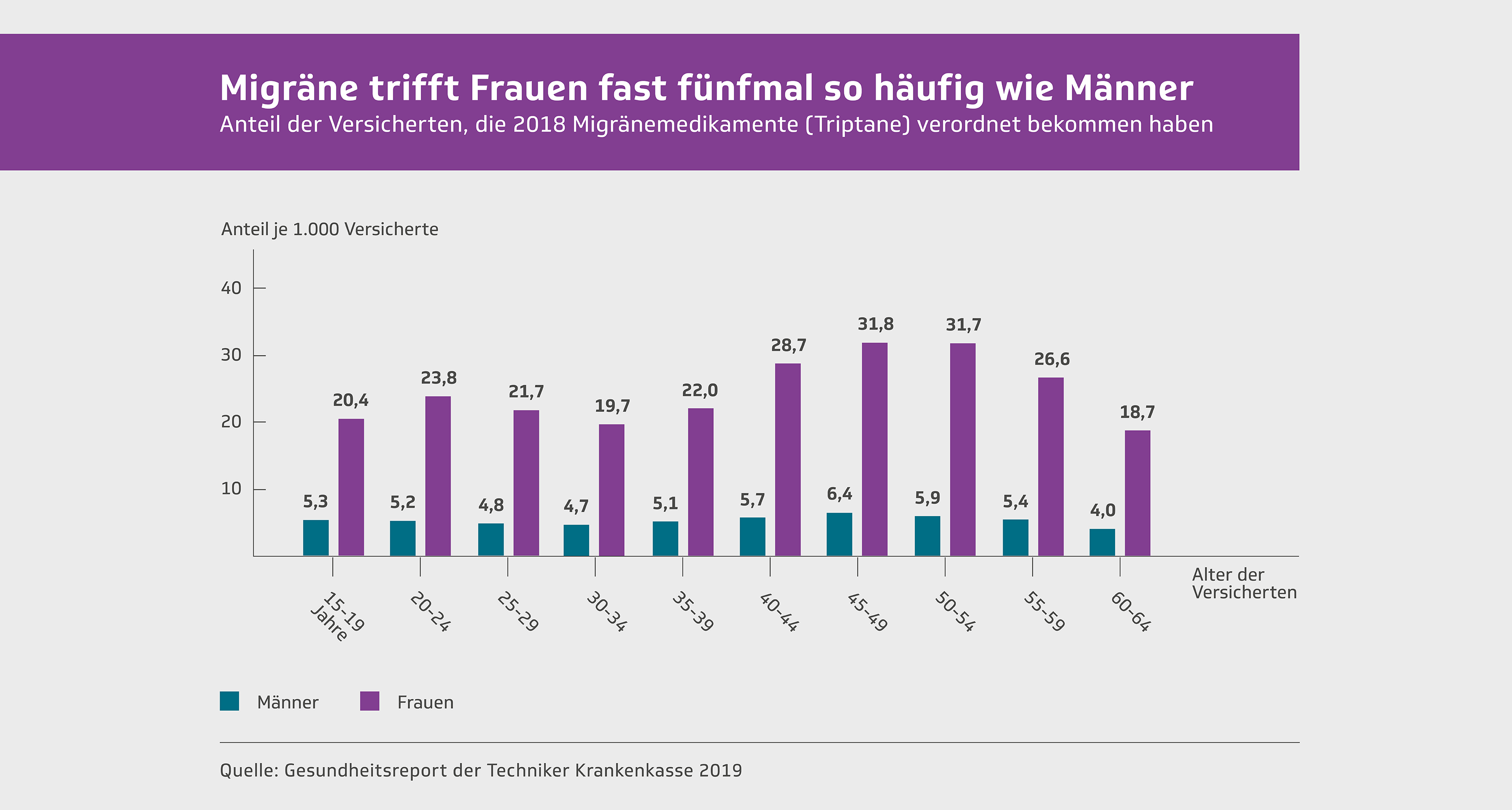
When it comes to migraines, there is a difference between the sexes not only in the frequency of occurrence, but also in the severity of the disease. This becomes clear when evaluating health insurance data regarding the use of healthcare. Such an approach makes it possible to say how many people suffer from their migraines to such an extent that they also incur costs. The BARMER Doctors' Report 2017 provides data for Germany with a focus on headaches (4). Accordingly, in 2015, a total of 2.1% of men were treated medically for migraines, while 6.8% of women were treated, i.e. 3.2 times as many. Among 24-year-olds and 50-year-olds, one in 10 women was affected. 4.3 times more women than men were prescribed triptans - specific migraine treatments that are only used when painkillers are no longer effective enough. In comparison to the sexes, women require more frequent and more intensive medical treatment than would have been expected based on the pure prevalence. Migraines are obviously more severe in women. This is also supported by the fact that the proportion of women in clinical studies on migraine is consistently disproportionate at 80 to 85% (5, 6). There is a high level of suffering and obviously an unmet need for new treatment options. (Katja Heinze-Kuhn, Axel Heinze and Hartmut Göbel).
Literature:
- Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache. 2013;53(2):230-46.
- Marmura MJ. Triggers, Protectors, and Predictors in Episodic Migraine. Curr Pain Headache Rep. 2018;22(12):81.
- Silberstein SD. Sex hormones and headaches. Rev Neurol (Paris). 2000;156 Suppl 4:4S30-41.
- Grobe T, Steinmann S, Szecsenyi J. BARMER doctor's report. Series of publications on health analysis, Volume 1: BARMER headquarters, Asgard Verlagsservice GmbH; 2017.
- Reuter U, Goadsby PJ, Lanteri-Minet M, Wen S, Hours-Zesiger P, Ferrari MD, et al. Efficacy and tolerability of erenumab in patients with episodic migraine in whom two-to-four previous preventive treatments were unsuccessful: a randomized, double-blind, placebo-controlled, phase 3b study. Lancet. 2018;392(10161):2280-7.
- Skljarevski V, Matharu M, Millen BA, Ossipov MH, Kim BK, Yang JY. Efficacy and safety of galcanezumab for the prevention of episodic migraine: Results of the EVOLVE-2 Phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38(8):1442-54.








Leave a comment